Page 1 :
NOTE – This is original work of Dr. Girish Waru., , Gynecology, S.N., 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 31, , Topic, Abnormal Uterine Bleeding, Dysfunctional Uterine Bleeding, Primary Amenorrhea, Secondary Amenorrhea, Premenstrual Syndrome, Primary Dysmenorrhea, Secondary Dysmenorrhea, Pelvic Masses, Menopause, Pelvic Inflammatory Disease, Trichomonal Vaginitis, Vulvo-vaginal Candidiasis, Mucopurulent Cervicitis, Pelvic Organ Prolapse, Fibroid Uterus, Atrophic Vaginitis, Post-menopausal Bleeding, Fractional Curettage, Endometriosis, Abdomino-pelvic Lump, Pap Smear, Morphological Abnormalities of Pap Smear, Laparoscopy in Gynecology, Cervical Cancer, Polycystic Ovarian Syndrome, Leucorrhoea, Abnormal Vaginal Discharge, Pruiritus Vulva, Pelvic Pain – Acute & Chronic, Methods of Contraception & IUCDs, , Page, 2, 4, 6, 7, 8, 9, 10, 11, 12, 14, 16, 17, 18, 19, 22, 25, 26, 27, 28, 30, 31, 32, 33, 35, 37, 39, 40, 41, 42, 43, , Page 1 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 2 :
Dr. Girish Waru – Gynecology, , AUB, , Chapter 1, , Abnormal Uterine Bleeding (AUB), Def., Any uterine bleeding outside the normal volume, duration, regularity or frequency is considered as abnormal, uterine bleeding., Normal menstruation, •, •, •, , Cycle interval, Menstrual flow, Menstrual Blood Loss, , - 28 days (21 – 35 days), - 4 – 5 days, - 35 ml (20 – 80 ml), , Common Causes of AUB, 1., 2., 3., 4., 5., 6., 7., 8., , Dysfunctional Uterine Bleeding (DUB), Infection, Endocrine Dysfunction (Thyroid Disorder), Pregnancy Complication, Hematological Disorder, Neoplastic Growth, Uterine Fibroids, Medication, , Patterns of AUB, A. Menorrhagia –, Cyclic bleeding at normal intervals; bleeding either more than 80 ml or more than 7 days or both., Cause, i., Fibroid Uterus, vii., Endocrinal, ii., Adenomyosis, - Hypothyroidism, iii., Pelvic Endometriosis, - Hyperthyroidism, iv., IUCD in Utero, viii., Hematological – Leukemia, v., Retroverted Uterus, ix., Emotional Upset, vi., DUB, x., Hypothalamo-Pituitary-Ovarian, Endometrial Axis, B., , Polymenorrhoea (Epimenorrhoea), Cyclic bleeding where cycle is reduced to an arbitrary limit of less than 21 days & remain constant, at that frequency., C. Metrorrhagia, Irregular acyclic bleeding from the uterus. Amount of bleeding is variable., D. Oligomenorrhagia, Menstrual bleeding occurring more than 35 days apart and which remain constant at that, frequency., E. Hypomenorrhoea, When the menstrual bleeding is unduly scanty and last for less than 2 days., , Page 2 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 3 :
Dr. Girish Waru – Gynecology, , AUB, , Signs & Symptoms, •, •, •, •, •, •, , Bleeding from uterine cavity on, Speculum Examination, Tachycardia, Anemia, Painless, but sometimes Pelvic Pain, occur, Dizziness, Abnormal Pelvic Mass., , Complication, 1., 2., 3., 4., , Dysparunia, Infertility, Anemia, Hypovolemic Shock., , Investigation, , , , , , , , , , , , , , CBC, Coagulation Profile (PT, PTT), Ultrasound – Pelvis & Abdomen, Pregnancy Test, Endometrial Sample to exclude Neoplasia, PAP Smear, Urinalysis, Saline Infusion Sonography – for Polyp Fibroid, Hysteroscopy, Laproscopy, Endometrial Biopsy, Diagnostic Uterine Curettage (D&C), , Management, A. Medical, a) Non-hormonal Therapy, o Mefanamic Acid – 500 mg PO TDS or, o Ibuprofen – 400 mg PO TDS x 3 days, b) Hormonal Therapy, i., Combined Oral Contraceptive Pills, ii., Progesterone Supplement (Suppositories, Injections, Pessaries), o Duphaston – 10 mg PO or 20 mg OD daily 11th to 25th of Menstrual, Cycle (M.C.), o Utrogetan 100 mg – Dose - 200 mg OD 16th to 25th day of M.C., o High dose long lasting Progestogen (Depo-Provera), B. Surgical, i., Endometrial Ablation, ii., Hysteroscopic Resection, iii., Polypectomy, iv., Myomectomy, v., Hysterectomy., …….xxx, Page 3 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 4 :
Dr. Girish Waru – Gynecology, , DUB, , Chapter 2, , Dysfunctional Uterine Bleeding (DUB), Definition, A state of abnormal uterine bleeding without any clinically detectable organic systemic & iatrogenic cause., Heavy menstrual bleeding is defined as a bleeding that interferes with woman’s physical, emotional, social, and maternal quality of life., Causes, 1. Ovular Bleeding (20 %), ▪ Polymenorrhea, ▪ Oligomenorrhea, ▪ Functional Menorrhagia., 2. Anovular Bleeding (80 %), ▪ Menorrhagia, ▪ Cyclic Glandular Hyperplastia, Incidence, •, •, •, •, , Pubertal or Adolescent DUB, Reproductive DUB, Perimenopausal DUB, Post-menopausal DUB, , - age < 20 yrs, - age 20 to 40 yrs, - age above 40 yrs, - incidence around, , -4%, - 57 %, - 39 %, - 10 %, , How to Make Diagnosis, A. H/o Abnormal Uterine Bleeding, i., Excessive Menses – duration of MC flow > 7 days or menstrual blood loss > 80 ml., ii., Frequent Menses – duration of MC < 21 days, iii., Irregular / Acyclic Uterine bleeding., B. H/o Symptoms suggestive of –, i., Pregnancy, ii., Dysmenorrhoea, iii., Infertility due to - Endometriosis & PID, Fibroid, Adenomyosis, iv., H/o Contraceptive Practice, HRT., Examination, •, •, •, •, , General exam – for sign of Anemia, Thyroid disease, Abdominal exam – for Masses, Speculum exam – to visualize Cervix, Vagina, Per Vaginal exam – for Uterine enlargement, Fibroid, PID, Endometriosis or Any Adnexal Mass., , Page 4 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 6 :
Dr. Girish Waru – Gynecology, , Primary Amenorrhea, , Chapter 3, , Primary Amenorrhea, Absence of menses at 14 yrs of age without secondary sexual development or age 14 with secondary, sexual development., Causes, 1., 2., 3., 4., , Hypothalamic-Pituitary Insufficiency, Ovarian Causes, Imperforated Hymen / Vaginal Septum, Chromosomal (Turner’s syndrome), , Signs & Symptoms, ▪, ▪, ▪, , Absence of menses at age 14 without secondary sexual development, Presence of secondary sexual character development and absence of menses at age 16., Absence or presence of Pelvic Pain, , Investigation, , , , , , , , , Progesterone Challenge Test, Hormonal Profile (FSH) & Karyotyping, Pregnancy Test, Ultrasonography – Pelvis, Thyroid test, X-ray Skull – Pituitary Tumor or Necrosis, CT Scan – Brain, , Management, 1. Hormonal ℞ (OC Pills), 2. Surgical ℞, -, , Hymenotomy – if imperforated hymen, Resection of Vaginal Septum, Tumor resection., , …….xxx, , Page 6 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 7 :
Dr. Girish Waru – Gynecology, , Secondary Amenorrhea, , Chapter 4, , Secondary Amenorrhea, Cessation or stopping of menstruation for a period equivalent to a length of 3 consecutive cycle or for 6, months., Causes, 1., 2., 3., 4., 5., 6., 7., 8., 9., 10., 11., , Pregnancy & Lactation, Menopause, Hypothalamo-Pituitary Inflammation / Neoplasm, Stress, Anxiety, Excessive Loss of Weight, Drugs (Danazol, Decopeplyl), Contraceptives, Chronic disease, Premature Ovarian Failure, PCOS., , Signs & Symptoms, •, •, •, •, •, •, •, , At least 3 consecutive cycle of absence of menses, Galactorrhoea, Premature menopause, Obesity, Headache, Polyuria, Polydipsia, , Investigation, , , , , , , Hormonal profile, Pregnancy test, USG – Pelvis, Thyroid test, X-ray Skull – Pituitary tumor., , Management, I., II., III., IV., , Hormonal Treatment – for PCOS, Surgical Treatment - Tumor resection, Weight loss, Normalize the BMI., , …..xxx, , Page 7 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 8 :
Dr. Girish Waru – Gynecology, , Premenstrual Syndrome, , Chapter 5, , Premenstrual Syndrome (PMS), PMS is a psychoneuroendocrine disorder of unknown etiology, often noticed just prior to menstruation., There is a cyclic appearance of large number of symptoms during the last 7 – 10 days of menstrual cycle., Symptoms, 1. Related to Water Retention, ▪ Abdominal bloating, ▪ Breast tenderness, ▪ Swelling of extremities, ▪ Weight gain, Neurological Symptoms, ▪ Irritability, ▪ Depression, ▪ Mood swings, ▪ Forgetfulness, ▪ Restlessness, ▪ Increased Appetite, Pathophysiology, , 2., , Behavioral Symptoms, ▪ Fatigue, ▪ Tiredness, ▪ Insomnia, ▪ Dysparenuia, , 3., , •, •, •, , ▪, ▪, ▪, ▪, ▪, ▪, , Tearfulness, Anxiety, Tension, Confusion, Headache, Anger., , Alteration in level of Estrogen & Progesterone, Excessive Serotonin & β Endorphins secretions, Exaggerated End Organ Response to the normal cyclic changes in Ovarian Hormones., , Management, A. Non-Pharmacological, ▪ Life style modification, ▪ Dietetic advice & Exercises, B. Non-Hormonal, ▪ Pyridoxine – 100 mg daily, ▪ Aplrazolam – 0.25 BD, ▪ Selective Serotonin Reuptake Inhibitors (SSRI), - Fluoxetine – 20 mg/day, - Sertaline – 50 mg/day, C. Hormones, ▪ Combined Oral Contraceptive Pills - suppression of Ovulation, ▪ LNG – IUD, - suppress Ovarian cycle, ▪ Danazol – 200 mg/ day, - suppression of ovarian cycle, ▪ GnRH Analogs for 6 months, - suppressed Gonadal steroids, ▪ Bromocriptine – 2.5 mg daily, - for Breast complaints., D. Surgical, ▪ Hysterectomy with bilateral Oophorectomy., ……..xxx, Page 8 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 10 :
Dr. Girish Waru – Gynecology, , Secondary Dysmenorrhea, , Chapter 7, , Secondary Dysmenorrhea, Secondary Dysmenorrhea is normally considered to be menstruation associated pain occurring in the, presence of pelvic pathology., Causes, 1., 2., 3., 4., 5., 6., 7., 8., 9., , Endometriosis, Adenomyosis, IUCD in utero, Cervical Stenosis, Pelvic Adhesion, Uterine Fibroid, Pelvic Congestion, Endometrial Polyp, Chronic Pelvic Infection, , Clinical Feature, •, •, •, •, •, , Dull Pain situated in back & in front without any radiation, Later in Reproductive life, Dyspareunia, It usually appears 3 – 5 day prior to M.C. & relieves with onset of bleeding., An Endometrial Polyp or Submucous Fibroid – usually occurring at the beginning of menstruation, cause pelvic lower abdominal pain., , Investigation, , , , , , , CBC, ESR, C-Reactive Protein, Vaginal Swab, USG, Laparoscopy, Hysteroscopy, , Management, NSAIDs – start 1 – 2 days before M.C., Mefenamic Acid 250 – 500 tds / Naproxen 250 6 hrly., Assurance, Keep Bowel empty., ……xxx, , Page 10 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 11 :
Dr. Girish Waru – Gynecology, , Pelvic Mass, , Chapter 8, , Pelvic mass, An abnormal structure or growth in the pelvic cavity arising from –, - Pelvic Organ – Ovaries, Fallopian Tubes, Uterus, Cervix, Bladder, Bowel, Peritoneum., - Metastatic from extra-pelvic structures such as Stomach, Breast, Lungs., Risk Factors, 1., 2., 3., 4., 5., 6., 7., 8., , Infertility, Family History of Breast / Ovarian / Colon Cancer., Pelvic surgery – Hematoma, Abscess, Appendicitis, Pelvic Inflammatory Disease, Endometriosis, Smoking, Pelvic Kidney – congenital abnormality., , Sign & Symptoms, •, •, •, •, •, •, •, •, •, •, •, •, •, , Pelvic pain, Fever, Vaginal discharge, Heaviness in abdomen, Pelvic mass, Abnormal Uterine bleeding, Dyspareunia, Dysmenorrhea, Infertility, Amenorrhea, DUB, Urinary Urgency or Retention, Cachexia in CA., , Investigation, , , , , , , , Pregnancy test, CBC, ESR, BSL, Urine Analysis, Renal function, CA 125, Pelvic USG, , HSG (Hysterosalphingography), Laparoscopy, Plain Abdominal X-ray, CT Scan & MRI, , Complication, • Torsion, • Compression, • Rupture, Management, , •, •, , Infertility, Malignancy transformation., , Laparoscopy & Laprotomy – for etiologic treatment of pelvic mass, Adjuvant Treatment – depending on the cause, - Hormones (OC Pills), - NSAIDs, - Radiotherapy & Chemotherapy for Malignant Disease., ……xxx, , Page 11 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 12 :
Dr. Girish Waru – Gynecology, , Menopause, , Chapter 9, , Menopause, Menopause means permanent cessation of menstruation at the end of reproductive life due to loss of, ovarian follicular activity. i.e. amenorrhea for 12 consecutive months without any other pathology at age of, 45 to 55 yrs., Pathophysiology, Diminished Estradiol production, ↓, Decreases Negative Feedback Effect on Hypothalo-Pituitary Axis resulting in increase in FSH and, LH & diminished inhibition ↓Prolactin., ↓, Estradiol production drop down, ↓, No Endometrial growth, ↓, Absence Menstruation, Organ Changes, Ovaries, Fallopian Tube, Uterus, Vagina, Vulva, Breast, , Shrink in size, Feature of Atrophy, Cilia disappear., Become smaller Body Cervix ratio 1:1, Endometrium – thin, atrophic, Cervical secretion – scanty, Become narrower due to loss of elasticity, Vaginal epithelium become thin, Vaginal pH become alkaline., Feature of atrophy, Labia flattened, Flat & pendulous., , Symptoms, A. Menstrual Changes, -, , Shorter cycles, Irregular bleeding, , D. Sexual Dysfunction, -, , B. Vasomotor Symptoms, -, , Hot flushes, Night sweat, Sleep disturbances, , E. Urinary, , Vaginal dryness, Dyspareunia, , -, , Incontinence, Urgency, Dysuria, , C. Psychological, -, , Irritability, Mood swings, Poor memory, Depression, , F. Other, -, , Back pain, Joint pain, Skin – Dryness, thinning, of skin, Hair – Loss of Head-Hair, increase or loss of body, hair, Osteoporosis & fracture., , Page 12 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 13 :
Dr. Girish Waru – Gynecology, , Menopause, , Investigation, Cessation of M.C. for consecutive12 months during climacteric, Average age of menopause – 50 yrs., Appearance of menopausal symptoms – hot flash and night sweat, Vaginal dryness, Serum Estradiol < 20 pg/ml, Serum FSH & LH > 40 mIU/ ml, Bone densitometory., Complication, •, •, , Pathological fracture, CVS disease., , Management, Non-Hormonal treatment, o Lifestyle medication, o Nutritious Diet, o Supplementary Calcium, o Vitamin D3 – 1500-2000 IU/day, o Exercise, o Cessation of Smoking & Alcohol, o Bisphosphonates, o Calcitonin, o Selective Estrogen Receptor Modulators (SERMs), o Clonidine ( agonist) for hot flushes, o Gabapentin for hot flushes, o Soya protein act as SERM, o Vitamin E reduce hot flushes (25 %), Hormone Therapy, It is indicated for short period of time only., o Relief of menopausal symptoms, o Relief of vasomotor symptoms, o Prevention of osteoporosis, o Premature ovarian failure, o Surgical & Radiation menopause., Estrogen Oral Patch or Gel form, Tibolone – 2.5 mg OD x 30 days., , , , Commonly used Estrogen & cyclic Progestin – for woman with intact Uterus., Estrogen given continuously for 25 days & Progestin is added for last 12 – 14 days., , Risk of Hormone Therapy, I., II., III., IV., V., VI., , Endometrial CA, Breast CA, DVT, Coronary Heart Disease, Gall Bladder Disease, Dementia, , …….xxx, , Page 13 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 14 :
Dr. Girish Waru – Gynecology, , PID, , Chapter 10, , Pelvic Inflammatory Disease (PID), PID is infection usually sexually transmitted disease often including any combination of inflammatory, disorder involving Uterus, Fallopian tubes, Ligament of the Uterus and sometimes Ovaries., Cause, Pathogens, , , , , , N. gonorrhea, Chlamydia trachomatis, Mycoplasma hominis, Gardnerella vaginitis., , Risk Factors, •, •, •, •, •, •, •, •, , Age < 20 years, Earlier age at 1st sexual intercourse, Multiple sexual partners, History of sexually transmitted disease, Induced abortion, IUD, HSG, Post-partum & Posr-abortum endometritis, , Sign & Symptoms, •, •, •, •, •, •, , Asymptomatic, Fever, Lower abdominal tenderness, Abnormal vaginal discharge, Abnormal genital bleeding, Dyspareunia, , Complication, o Infertility, , o Ectopic pregnancy, , o Tubo-ovarian Abscess, , o Pelvi-peritonitis, , o Pelvic Abscess, , Investigation, Laboratory, - Leucocytosis with Neutrophilia, - ↑ESR, Culture & Sensitivity of Blood, Pus or Vaginal discharge., Vaginal Swab – evidence of Cervicitis, USG – evidence of inflammatory collection or abscess, Laproscopy – visualization of hyperemic tubes, purulent discharge., Endometrial biopsy, , Page 14 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 16 :
Dr. Girish Waru – Gynecology, , Trichomonal Vaginitis, , Chapter 11, , Trichomonal Vaginitis, Trichomonal vaginitis is an inflammation of Vagina & Vulva, Cause, , , Trichomonas vaginalis, , Signs & Symptoms, •, •, •, •, , Dysuria, Foul smelling, frothy vaginal discharge, noticeable several days after M.C., Vaginal itching & Pain, Redness of Vaginal Lips & Vagina, , Complication, Premature birth, Low birth weight, , ▪, ▪, , Investigation, Microscopic Examination of Saline Wet Mounted Preparation, Litmus Test for pH of Vaginal secretions, Management, Metronidazole – 500 mg PO BD x 7 days, Metro Gel 0.75% - 5 gm Intra-vaginally OD x 5 days., OR, Clindamycin – 300 mg PO BD x 7 days, OR, Tinidazole – 2 gm Single Dose, , , , , , In pregnancy, Metronidazole 2 gm PO single dose, Advise sexual abstention until symptoms improve., Avoid Alcohol during treatment with Oral Metronidazole for 24 hrs; thereafter last dose., Treatment of Partner also advised., , ……xxx, , Page 16 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 19 :
Dr. Girish Waru – Gynecology, , Pelvic Organ Prolapse, , Chapter 14, , Pelvic Organ Prolapse, Pelvic organ prolapse is a common gynecological problem in woman above the age of 40 yrs., Types of Genital Prolapse, 1. Vaginal, a. Anterior wall, - Cystocele, (upper 2/3), - Urethrocele, (lower 1/3), - Cystourethrocele, b. Posterior wall, - Relaxed Perineum, - Rectocele, - Enterocele (upper 1/3), - Secondary Vault propalse (after Hysterectomy), 2. Uteru-vaginal, - Prolapse of Uterus, Cervix, Upper Vagina, - Cystocele occur first followed by traction effect on Cervix, cause retroversion of Uterus, - Pushing it down into vagina, 3. Congenital, - No Cystocele., - Uterus herniated down with inverted Vagina., Degree of Uterine Prolapse, a. Normal, - External OS lies at level of Ischeal Spine, - No prolapse, b. 1st Degree, - Uterus descends down from its normal anatomical position, but External OS still remain, above the introitus, c. 2nd Degree, - External OS protrudes outside the vaginal introitus, - Uterine body is still remain inside vagina, d. 3rd Degree, - Cervix, Body & Fundus descend to lie outside the introitus, e. Procidenta, - Involves prolapse of Uterus with eversion of entire vagina., Symptoms, A. Lower Urinary Tract Symptom, - Incomplete Empting, - Recurrent UTI, frequency, Nocturia, - Stress Urinary Incontinence, - Voiding difficulty,, - May require reduce prolapse, before passing urine., , B. Bowel, Symptoms, - Constipation, - Straining, - Incomplete, evacuation, , C. Sexual Symptoms, , D. Others, , - Interference with, sexual activity, - Dyspareunia, - Decreased sexual, desire, , -, , Pelvic pressure, Heaviness, Pain, Presence of vaginal, bulge & mass, - Low back pain, , Page 19 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 20 :
Dr. Girish Waru – Gynecology, , Pelvic Organ Prolapse, , Signs, •, •, •, •, •, , P/A, - look for mass or lump, Local Exam, - inspection of Vulva with coughing & straining, demonstrate severe prolapse, Sim’s Speculum Exam, - see degree of prolapse & type of prolapse, Vaginal Exam, - Uterine size, position, Adnexal mass, Rectal Exam, - differentiate Rectocele from Enterocele., , Predisposing Factors, 1., 2., 3., 4., , Injuries to support organ during childbirth, Obesity, chronic cough, chronic constipation, Atrophy & loss of tone due to aging, Estrogen deficiency., Congenital weakness of tissue can lead nulliparous prolapse., , Management, 1. Preventive, , 2. Conservative, , 3. Surgery, , Preventive Management, a. Adequate Antenatal & Intranatal Care, o To avoid injury to supporting structure during time of vaginal delivery, b. Adequate Postnatal Care, o To encourage early ambulance, o To encourage pelvic floor exercise Kegel Exercise, c. General Measures, o To avoid strenuous activities, chronic cough & constipation, heavy weight lifting., Conservative Management, Indication, •, •, •, •, , Asymptomatic women, Old Woman not willing surgery, Mild degree prolapse, Prolapse in early pregnancy., , Management, o, o, o, o, , Avoid strenuous activities – cough, constipation, Estrogen replacement may improve minor degree prolapse in postmenopausal women, Pelvic floor exercise in an attempt to strengthen the muscle – Kegel exercise, Pessary Treatment – relieve symptoms by streaching hiatus urogenitalis. Thus preventing, vaginal & uterine descent., , Indication for Pessary Treatment, , , , , , Early pregnancy upto 18 weeks, place inside, Puerperium to facilitate involution, Patient unwilling for operation, While waiting for operation., , Surgical Management of Prolapse, •, , Surgery is the treatment of symptomatic prolapse where conservative management has failed or is, not indicated., , a. Restorative, Correcting her own support tissue, Compensatory – using permanent graft material., Page 20 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 21 :
Dr. Girish Waru – Gynecology, , Pelvic Organ Prolapse, , b., , Extirpative, Removing Uterus & correcting the support tissue, c. Obliterative, Closing the vagina (Colpoclesis), Meticulous Examination even under anesthesia is necessary to establish the correct diagnosis of, organ prolapsed, so that effective & appropriate repair can be carried., There is no single procedure for all types of prolapse., Pelvic Organ Prolapse with Stress incontinence, 1. Vaginal, 2. Abdominal, , - Transobturator type procedure (TOT operation), - Bruch operation., , ……..xxx, , Page 21 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 22 :
Dr. Girish Waru – Gynecology, , Fibroid Uterus, , Chapter 15, , Fibroid Uterus / fibromyoma / leiomyoma Uterus, Fibroid is the most common benign tumor of the uterus., This is composed of smooth muscle & fibrous connective tissue , so also called as leiomyoma, myoma,, fibromyoma., Incidence, •, •, , 20 % of woman at age of 30, Prevalence is highest between 35 to 45 yrs., , Risk factors, , , , , , , , , Reduced Risk Factor, , , , , , Nulliparity, Obesity, ↑ BMI, PCOS, Hyperestrogenic state, High Fat diet, Family history., , Multiparity, Menopause, OC Pills use, Smoking., , Types, 1. Body, , 2. Cervical, , Body, ▪, ▪, ▪, , Cervical, Interstitial (Intramural), Subserous –, - Parasitic, - Pseudo, Submucous - Sessile, - Polyp, , - 75 %, - 15 %, , •, •, •, •, •, •, •, , Anterior, Posterior, Central, Lateral, , -5%, , Symptoms of Fibroid Uterus, •, •, , ▪, ▪, ▪, ▪, , Asymptomatic – majority 75 %, Menstrual abnormality – Menorrhagia /, Metrorrhagia, Dysmenorrhoea, Dyspareunia, Subfertility, Pressure symptoms, Recurrent, Pregnancy, Loss, –, Miscarriage / Preterm Labor, Lower abdominal or Pelvic Pain, Abdominal enlargement., , Secondary Changes in Fibroids / Complication, ▪, ▪, ▪, ▪, ▪, ▪, ▪, ▪, ▪, ▪, , Hyaline degeneration - most common, 65 %, Cystic degeneration, Fatty degeneration, Calcific degeneration, Red degeneration, Atrophy, Necrosis, Infection, Vascular changes, Sacromatous changes (less than 0.1 %, cases), , Page 22 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 23 :
Dr. Girish Waru – Gynecology, , Pelvic Pathologies Commonly Co-existent, with Fibroid, ➢, ➢, ➢, ➢, ➢, ➢, , Fibroid Uterus, , Differential Diagnosis, , Endometrial Hyperplasia, Endometrial Polyps, Endometriosis, Anovulation & DUB, Pelvic Inflammatory disease (PID), Tubal Pregnancy., , ▪, ▪, ▪, ▪, ▪, ▪, , Adenomyosis, Bicornuate Uterus, Ovarian tumor, Retroperitoneal tumor, Full Bladder, Pregnancy, , Investigation, USG & Color Doppler (TVS), - Uterine contour is enlarged & distorted, - Vascularization is at periphery of fibroid, - Central vascularization indicate degeneration, Saline Infusion Sonography, MRI, Laproscopy – useful of uterine size less than 12 week, Hysteroscopy, HSG, Uterine Curettage, CBC, Blood Group, Urine analysis, PAP Smear, Endometrial Biopsy – when diagnosis in doubt., Management, A. Asymptomatic Management, •, , Fibroid detected accidentally on routine exam for complaints other than Fibroids, 1. Observation, - Size < 12 weeks (of pregnancy size of uterus), - Diagnosis certain, - Follow up at interval of 6 month & USG if grow in size, Surgery is indicated., , B. Symptomatic Management, 1. Levonorgestrel Releasing Intra-uterine System, - For small Fibroid, not destroying Uterine Cavity, 2. Tranexamic Acid – Meorrhagia, 3. NSAIDs – Menorrhagia, Dysmenorrhoea, 4. Oral Progestogen (Norethisterone) – size reduction, 5. Injected Progestogen – size reduction, 6. GnRH Agonist Administration., For, - Preoperatively to shrink fibroid & decrease Anemia, - Short term treatment for Alternative to Surgery in perimenopausal female, - Tab Danazol has been associated with reduction in volume of fibroid by 20 – 25 %, Disadvantages of GnRH Agonist, - High cost, - Hot flushes, - Vaginal Dryness, - Risk of Osteoporosis, Page 23 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 24 :
Dr. Girish Waru – Gynecology, , Fibroid Uterus, , C. Surgical Management, Hysterectomy, - Abdominal / Vaginally / Laproscopically, Myomectomy, - Removal of Myomas while Uterus is preserved., Merit, -, , Preservation of Fertility, but recurrence of fibroid,, More in patient age less than 40 yrs., , ……xxx, , Page 24 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 25 :
Dr. Girish Waru – Gynecology, , Atrophic Vaginitis, , Chapter 16, , Atrophic Vaginitis (Senile Vaginitis), Vaginitis in postmenopausal women is called atrophic vaginitis, Cause, , , , , Estrogen deficiency, Vaginal defence lost, Vaginal mucosa is thin & more susceptible to infection, , Clinical Features, •, •, •, •, •, , Yellowish or blood stained vaginal discharge, Discomfort, Dryness in vagina & vulva, Soreness in the vulva, Dyspareunia, , On Examination, ▪, ▪, ▪, , Evidence of Pruritus vulvae, Vaginal examination is painful &, The walls are found inflamed, , Treatment, , , , , , , Improvement of general health, Treatment of infection, Systemic Estrogen therapy if no contraindication, Intra-vaginal Application of Estrogen cream, Good hygiene maintained., , ………xxx, , Page 25 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 26 :
Dr. Girish Waru – Gynecology, , Post-menopausal Bleeding, , Chapter 17, , Post-menopausal Bleeding, Bleeding per vagina following established menopause is called postmenopausal bleeding., Cause, , , , , , , , , , , , , Senile Endometriosis, Atrophic Endometrium, Endometrial Hyperplasia, DUB, Genital Malignancy – Cervix, Endometrium, Vagina., Uterine Polyp, Tubercular Endometritis, Cervical Erosion & Polyp, Senile Vaginitis, Decubitus ulcer., Retained & Forgotten foreign body such as Pessary or IUCD., , Investigation, , , , , , , , , USG Pelvis, Saline Infusion Sonography, Hysteroscopic exam, Endometrial Biopsy, Fractional Curettage, Laproscopy, CT & MRI, , Treatment, If cause is found, treatment of it, In recurrence or continued bleeding –, - Laprotomy – Hysterectomy with bilateral Salpingo-oophorectomy., …….xxx, , Page 26 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 27 :
Dr. Girish Waru – Gynecology, , Fractional Curettage, , Chapter 18, , Fractional Curettage, It is definite method of diagnosis of gynecological CA and can detect the extent of growth. This is done, under anesthesia with utmost gentleness., Steps, 1., 2., 3., 4., 5., 6., , Endocervical curettage (ECC), To pass an Uterine Sound to note the length of the Uterocervical Canal, Dilatation of Internal OS, Uterine Curettage at the fundus & lower part of the body., Finally a Polyp Forceps is introduced in case of any endometrial polyp has escaped the curette., Specimens so obtained should be placed in separate Container, labeled properly & submitted for, Histological exam., , Result of endometrial biopsy correlate well with endometrial curetting ., Endometrial biopsy (EB) is accurate to detect cancer in 91 – 99 %, Where EB is not possible due to Cervical Stenosis, followed up by dilatation & curettage (Fractional, Curettage), …….xxx, , Page 27 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 28 :
Dr. Girish Waru – Gynecology, , Endometriosis, , Chapter 19, , Endometriosis, Presence of functioning endometrium (gland and stroma) in site other than Uterine Mucosa is called, endometriosis., Sites, , , , , , , , , , , , Pelvic endometriosis, Pelvic Peritoneum, Abdominal viscera, Rectovaginal septum, Umbilicus, Abdominal Scar, Episiotomy scar, Vagina, Cervix, Lymph nodes, Distant site (Lungs, Pleura, Skin, Ureter, etc), , Risk Factors, ▪, ▪, ▪, ▪, ▪, ▪, , Low parity, Delayed child bearing, Family history of Endometriosis, Genital tract obstruction, Environmental toxin, Molecular defects, (Tumor Necrosis factor, Estrogen, Macrophages), , Symptoms, •, •, •, •, •, •, •, •, •, •, , Dysmenorrhoea – 70 %, Abnormal menstruation – 20 %, Infertility, Dyspareunia, Chronic pelvic pain, Abdominal pain, Urinary frequency, dysuria, Hematuria, Diarrhoea, Constipation, Rectal bleeding , Melena, Chronic fatigue, Hemoptysis (rarely), , Investigation, Clinical Diagnosis, Speculum Exam –, - Bluish powder burn lesion may be seen on Cervix, Bimanual Exam –, - Reveal nodularity in pouch of Douglas, nodular feel of the uterosacral ligaments, fixed, Retroverted uterus, unilateral or bilateral Adnexal mass (Chocolate Cysts), Serum Marker, - Cancer Antigen – CA 125, USG, MRI, CT Scan, Page 28 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 29 :
Dr. Girish Waru – Gynecology, , , , , , , Endometriosis, , Colonoscopy, Retrosigmoidoscopy, Cystoscopy, Laproscopy, Biopsy confirmation, Intravenous Urology – if renal involvement., , Complications, 1., 2., 3., 4., , Endocrinopathy – Infertility, Malignancy., Rupture of Chocolate Cyst, Infection of Chocolate cyst, Obstruction – Intestine, Urethral, , Staging, •, •, •, •, , Stage I - Minimal, Stage II - Mild, Stage III - Moderate, Stage IV - Severe, , -1–5, - 6 – 15, - 16 – 40, - > 40, , Management, 1. Expectant Treatment (Observation only), ▪ With NSAIDs – for pain, ▪ Married women are encouraged to have Conception, ▪ Pregnancy usually cures the condition., 2., , Hormonal Treatment, ▪ Aim of Hormonal treatment is to induce atrophy of the Endometriotic implant., ▪ It is suppressed rather than curative., Treatment, a) By producing Pseudo-pregnancy by Combined Oral Pills, b) By producing Menopause by Danazol, c) By producing Medical Oophorectomy by GnRH Agonists., ▪, , 3., , The hormones used are gratifying in superficial peritoneal implant & endometriomas of, less than 1 cm., , Surgical Management, a) Conservative Surgery, Laproscopic Method, i., Cauterization, ii., Laproscopic Uterosacral Nerve Ablation, iii., Excision of Retro-vaginal Nodules, iv., Endometrioma – Aspiration Cystectomy., b) Definitive Surgery, Laproscopy / Lapratomy, i., Hysterotomy with bilateral Salingooophorectomy, ii., Resection of Bowel or Ureter – may be needed., , …….xxx, , Page 29 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 30 :
Dr. Girish Waru – Gynecology, , Abdomino-pelvic Lumps, , Chapter 20, , Abdomino-pelvic Lumps, 1 Toddler’s (< 5 yrs), , • Ovarian tumor, • Full Bladder, , 2 5 yrs to age of Puberty, , • Ovarian tumor, • Full Bladder, , 3 Child Bearing Period, , •, •, •, •, •, •, •, •, •, , Pregnancy, Full Bladder, Ovarian Tumor, Fibroid, Adenomyosis, Chocolate Cyst, Pelvic Hematocele, Pelvic Abscess, Encysted Peritonitis, , 4 Post-menopausal Period • Ovarian tumor, • Pyometra, • Sarcoma Uterus, ……xxx, , Page 30 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 31 :
Dr. Girish Waru – Gynecology, , PAP Smear, , Chapter 21, , PAP Smear, Cervical and vaginal smear for Exfoliative cytology., Indication, 1. As a Screening procedure, 2. For Cyto-hormonal study, 3. Others., Screening Procedure, A. Collection of Material, ▪ Cervix is exposed with a Cusco’s Vaginal Speculum without Lubricant & prior to Bimanual, exam., B. Cervical Scraping, ▪ Material from the cervix is best collected using Ayre’s Spatula, made of wood or plastic., ▪ Whole of the Squamocolumnar junction has to be scraped to obtain good material., C. Vaginal Pool Aspiration, ▪ Collection by any one of the method should be combined with endocervical sampling, either by Cytobrush or with moist Cotton Tip applicator., Fixation and Staging, •, •, •, •, , The principle of the staining is to achieve clear nuclear definition and to define cytoplasmic, coloration., The material so collected should be immediately spread over microscopic slide and at once put into, fixative ethyl alcohol (95 %) before drying., After fixing for about 30 minute, the slide is taken out, air dried and sent., It is stained with Sorr’s Method and examined by Cytologist., , Screening Program, 1 Low Risk, , 2 At, Average, Risk, , 3, , High, Risk, , Screening Program, , Screening Schedule, , • Woman who had never been sexually, active, • Women aged 65 or 70 who had 3, Negative Smears in past 10 yrs., • Woman who had Hysterectomy for, benign lesion., • Women between age 20 – 29, • Age > 30 yrs, , Nil, , • Age 65 to 70 yrs, , •, •, •, •, •, , Women with prior C1N2, C1N3, Oral pill users, Multiple Sexual Partners, Human Papilloma Virus Infection, Women who are Immunosuppressed, (HIV Positive), , PAP testing every 2 yrs, Every 3 yrs if previous 3 consecutive, smears are Negative, Stop screening, provided previous 3, consecutive smear were Negative in last, 10 yrs., Annual Screening for at least 20 yrs., , ………xxx, Page 31 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 32 :
Dr. Girish Waru – Gynecology, , Morphological Abnormalities of PAP Smear, , Chapter 22, , Morphological Abnormalities of PAP Smear, Morphological Abnormalities of Nucleus (Dyskaryosis), ➢, ➢, ➢, ➢, ➢, ➢, , Disproportionate Nuclear enlargement, Irregularity of Nuclear outline, Abnormalities of Nucleus in number, size, shape., Hyperchromasia, Condensation of Chromatin material, Multinucleation., , Abnormal Cells are –, Morphology, , Description, , 1 Mild Dyskaryosis, , ▪ Superficial Squamous Cells, , 2 Moderate, Dyskaryosis, , ▪ Intermediate or Superficial Squamous Cells, , 3 Severe Dyskaryosis, , ▪ Cells are Basal type, Oval, Polygonal or elongated in shape, , 4 Koilocytosis, , ▪ Nuclear abnormalities associated with human papilloma virus infection., ▪ Cells show typical central clearing with peripheral condensation of, cytoplasm., , 5 Carcinoma in situ, , ▪ Cells are parabasal type with increased nuclear cytoplasmic ratio., ▪ Cytoplasm is scanty., , 6 Invasive Carcinoma, , ▪ Cells are single or grouped in clusters., ▪ Cells show irregular nuclei & clumping of nuclear chromatin., ▪ Large tadpole cells are seen., , ……xxx, , Page 32 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 34 :
Dr. Girish Waru – Gynecology, , Laproscopy, , Contraindication of Laproscopy, •, •, •, •, •, •, •, , Severe Cardiopulmonary disease., Patient Hemodynamically unstable, Generalized Peritonitis, Intestinal Obstruction, Large Pelvic tumor, Pregnancy > 16 weeks, Advanced Malignancy., , Advantages of Laproscopic Surgery., 1., 2., 3., 4., 5., 6., 7., , Rapid postoperative recovery, Short Hospital Stay, Less Adhesion formation, Minimal Abdominal Scar, Reduce Blood loss, No Large incision, Less risk of Incisional Hernia., , ……xxx, , Page 34 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 35 :
Dr. Girish Waru – Gynecology, , Cervical Cancer, , Chapter 24, , Cervical Cancer, Cancer of Cervix is caused by mainly by Human Papilloma Virus (HPV), most common in female cancer in, developing countries and can be prevented by screening and vaccination against HPV., Gross Pathology, 1. Ectocervix, 2. Endocervix, , - 80 %, - 20 %, , Histopathology, •, •, •, •, , Squamous Cell Carcinoma, Adenocarcinoma, Adenoma Malignum, Neuroendocrine tumors., , Staging, Stage, , Invasive Carcinoma, , Stage 0, , Carcinoma in situ, , Stage I a1, , Stromal invasion < 3 mm, , Stage I a2, , Stromal invasion 3 – 5 mm, , Stage I b1, , Stromal invasion > 5 mm & < 4 cm, , Stage I b2, , Gross Cervical lesion > 4 cm, , Stage II a, , Extending to Upper 2/3 Vagina, , Stage II b, , With Obvious Parametrial Invasion, , Stage III a, , Extending to Lower ½ Vagina, , Stage III b Extending into Parametrium, Stage IV a, , Extending to Bladder / Bowel, , Stage IV b, , Distant Metastasis., , Cause / Risk Factors, , , , , , , , Infection with HPV, Early age of first sexual intercourse, Multiple sexual partners, Multiparity, Smoking, Age > 35 to < 45 yrs., , Signs & Symptoms, •, •, •, •, •, •, •, •, •, •, , Very often asymptomatic in early stages, Abnormal vaginal bleeding, Post-coital bleeding, Foul smelling vaginal discharge, Symptoms of metastasis, By Speculum Exam – lesion infiltrating, the Cervix, Pelvic pain, Leg oedema, Bladder symptoms, Rectal involvement – diarrhoea, PR, bleeding., , Page 35 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 36 :
Dr. Girish Waru – Gynecology, , Complication, ▪, ▪, ▪, ▪, ▪, ▪, ▪, ▪, , Anemia, Cachexia, Hemorrhage, Hematuria & Dysuria, Urethral Obstruction & Renal failure, Pyometra, Vesicovaginal fistula, Rectovaginal fistula., , Cervical Cancer, , Investigation, For invasive cancer, consider stage of, cancer., Speculum Exam – cervical lesion that, easily bleed on contact., PAP smear, VIA, VILI, HPV / DNA testing, Colposcopy, Biopsy, CBC & ESR, Renal function test, Intravenous Pyelography, X-ray Chest, Skeletal X-ray., CT scan, MRI Lymphatic Metastasis, PET, Proctoscopy., , Management, Principle of treatment, 1) Provide general supportive care, e.g. – correction of Anemia, 2) Undertake Exam under Anesthesia, e..g. – for staging & biopsy, 3) Provide supportive treatment, e.g. – Surgery and Radiotherapy according to Staging., General Measures, It is important to clinically assess the extent of disease prior to the onset of treatment, Surgery can be utilized in early stage of disease – Ia1 – IIa stage., Radiotherapy + chemotherapy can be utilized in all stages – I to IV., Surgery –, a) Stage Ia1, ▪ Cold Knife Cone or LEEP Cone - In young patient, ▪ Old woman – Hysterectomy, b) Stage Ib1, Ib2, IIa, ▪ Radial Hysterectomy with bilateral pelvic lymphadenectomy, c) Stage III & IV, ▪ Inoperable (Radiotherapy), , , , , , , Recommendation, , , , , , , HPV vaccine, Cervical Cancer Screening – PAP smear, Treatment of Precancerous lesion, Treatment of Invasive Cancer – Radiotherapy, Surgery, Chemotherapy, Psychological & Financial support in advanced form of Cervical Cancer., , ……..xxx, , Page 36 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 37 :
Dr. Girish Waru – Gynecology, , PCOS, , Chapter 25, , Polycystic Ovarian Syndrome (PCOS), Syndrome manifested by amenorrhea, hirsutism and obesity associated with enlarged polycystic ovaries., Most common endocrine disorders in woman of reproductive age., Pathology, •, •, •, , Typically the Ovaries are enlarged., Ovarian volume is increased, stroma is increased, capsule is thickened and pearly white in color., Presence of multiple follicular cysts, measuring about 2 – 9 mm in diameter, are crowded around, cortex., , Clinical Features, •, •, , •, •, •, , Obesity – abdominal, (50 %), Menstrual abnormalities (70 %), - Oligomenorrhea, - Amenorrhea, - DUB, - Infertility, Presence of Hirsutism, Acne, Acanthosis nigricans, - It is due to Insulin resistance, - Skin is thickened & pigmented (gray brown), - Commonly affected sites are nape of neck, inner thighs, groin, axilla., , Investigation, USG - TVS (Transvaginal Sonography) in Obese patient., Serum, - LH level - raised, - Estradiol & Estrone - raised, - SHBG level – reduced, - Hyperandrogenism, - Testosterone - raised, Insulin resistance, - Raised Fasting Insulin Level, Lipid profile, Laproscopy., Management, It need individualization of patient, It depends on her presenting symptoms like menstrual disorders, infertility, obesity, hirsutism or, combined symptoms., Treatment is primarily targeted to --1. Correct Biochemical Abnormalities like ▪ Hyperandrogenemia, ▪ Hyperinsulinemia, ▪ Hyperlipidemia, ▪ High Serum estrogen, ▪ Hypersecretion of LH, ▪ Low FSH, Page 37 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 39 :
Dr. Girish Waru – Gynecology, , Leucorrhea, , Chapter 26, , Leucorrhea, Leucorrhea is strictly defined as an excessive normal vaginal discharge., •, •, •, , The excess secretion is evident from persistent vulvar moistness or staining of undergarments, brownish yellow on drying, It is non-purulent & non-offensive, It is non-irritant & never causes pruritis., , Pathophysiology, ▪, ▪, , Normal vaginal secretion, The excessive secretion is due to –, a. Physiological Excess – When estrogen level is high, During Puberty, During Menstrual Cycle, - Around Ovulation, - Premenstrual, - Pregnancy, - During sexual act, b. Cervical cause, Cervical ectopy, Chronic cervicitis, Mucus polyp, c. Vaginal cause, Uterine prolapse, Retroverted uterus, Chronic PID, Pill use, Vaginal adenosis, , Treatment, Improvement of general health, Cervical factor, - Electrocautery, - Cryosurgery, Pelvic Lesion, - Appropriate therapy for pathology, Pill uses, - Stop pill temporarily, Treatment of Specific Condition., …….xxx, , Page 39 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 40 :
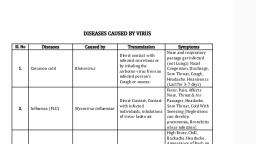
Dr. Girish Waru – Gynecology, , Abnormal Vaginal Discharge, , Chapter 27, , Abnormal vaginal Discharge, SN Cause, , Disease, , Description, , 1, , Infective, , •, •, •, •, , ➢, ➢, ➢, ➢, , 2, , Atrophic, , • Postmenopausal, , ➢ Discharge not prominent, ➢ Irritation is prominent, , 3, , Foreign, body, , • Forgotten Pessary, • Mechanical irritation, , ➢ Offensive, copious, ➢ Blood stained, , 4, , Chemical, , • Douches, Deodorants, • Contact dermatitis, , ➢ Soreness is more than, discharge., , 5, , Excretion, , ➢ Offensive with Pruritis, , 6, , Neoplasm, , • Contamination with Urine, feces cause, Secondary Vaginitis, • Fibroid, Polyp, • Genital malignancy, , Trichomonas vaginitis, Monilial vaginitis, Bacterial vaginosis, Cervicitis, , Frothy yellow, Curdy white, Gray white, fishy odor, Mucoid discharge, , ➢ Serosanguinous, ➢ Often offensive., , Investigation, Wet film for, - Trichomonas vaginalis, - Clue cells, KOH Test – Whiff test, - fungus, Discharge for Gram Staining, PAP smear, Urine Analysis & Culture sensitivity, HIV test., Blood tests for PID, ……..xxx, , Page 40 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 41 :
Dr. Girish Waru – Gynecology, , Pruritus Vulvae, , Chapter 28, , Pruritus Vulvae, •, , About 10 % of patient attending the Gynec. clinic, complain of vulvar itching., , Mechanism of Itching, 1. Spread Sensory innervations of the area, 2. Underlying vascular instability (greatly influenced by Emotions and result in production of, Histamine-like substance → induction of Itching., 3. Aggravation at Night because –, - Absence of distraction of mind, - Tired Central Nervous System, - Local Warmth & Lack of aeration., Etiology, , , , , , , , , Vaginal discharge, Local skin lesion, - Psoriasis, Dermatitis, Intertrigo, Infection of Vulva, - Fungal → Candida, - Viral → Herpes genitalis, genital warts, - Parasite →Scabies, Pediculosis, - STD → Gonorrhea, Trichomoniasis, Allergy or Contact Dermatitis, Non-Neoplastic Epithelial Disorder of Vulva, Neoplastic Epithelial disorder, - CA Vulva., , Treatment, Local Hygiene / Loose fitting Undergarments, Local Application of Antibiotics / Antifungal, To treat Specific Etiological factors – Local or systemic ℞, ……xxx, , Page 41 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 42 :
Dr. Girish Waru – Gynecology, , Acute Pelvic Pain, , Chapter 29, , Acute Pelvic Pain, SN, , Condition, , Cause, , 1, , Hemoperitoneum, , •, •, •, , Disturbed (ruptured) Tubal Pregnancy, Ruptured Chocolate Cyst, Ruptured Follicular Cyst, , (Peritoneal irritation), , •, •, , Acute PID, Tubo-ovarian Abscess, , 3, , Chemical Irritation, , •, , Following HSG, , 4, , Uterine Cramps, , •, •, , Abortion, Dysmenorrhoea, , 5, , Vascular complication with, Neurological involvement, , •, , Axial Rotation of Ovarian Tumor or Pedicle, , 6, , Visceral Distention, , •, •, •, , Intra-cystic haemorrhage, Hemotometra, Pyometra, , 7, , Non-gynecological, , •, •, •, •, •, , Appendicitis, UTI, Calculus, Intestinal Obstruction, Pancreatitis, Rectus sheath Hematoma., , (Peritoneal irritation), 2, , Infection, , Gynecological Chronic Pelvic Pain, Cyclic, 1, Intermenstrual pain, 2, Dysmenorrhea, 3, Premenstrual Syndrome, 4, Pelvic Congestion Syndrome, 5, Endometriosis, 6, Adenomyosis, 7, Ovarian Remnant Syndrome, , Acyclic, 1, Endometriosis, 2, PID, 3, Uterine Retroversion, 4, Uterine Prolapse, 5, Uterine Fibroid, 6, Ovarian Cyst, 7, Pelvic Adhesion Disease secondary to PID, 8, Intrauterine Device, 9, Pelvic Varicosities, 10 Psychosomatic, , Investigation, , , , , , , Routine Blood & Urine Test, Pregnancy Test, USG / X-ray Abdomen, CT –scan & MRI, Laproscopy., , ……..xxx, Page 42 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 43 :
Dr. Girish Waru – Gynecology, , Method of Contraception & IUCDs, , Chapter 30, , Methods of Contraception, A. Temporary, 1. Barrier method, 2. Natural Contraception, 3. Intrauterine Contraceptive Devices (IUCD), 4. Steroidal Contraception, B. Permanent, 1. Female – Tubal Occlusion, 2. Male – Vasectomy., , IUCDs, Intrauterine Contraceptive Devices, 1. Non-medicated, ▪ Lippe’s Loop, 2. Medicated (bioactive), ▪ CuT – 200, ▪ CuT – 380A, ▪ Multiload 250, ▪ Multiload 375, 3. Hormone Containing IUDs, ▪ LNG - IVS, Mode of Action, 1) Biochemical & Histological changes in Endometrium., 2) There may be increased Tubal Mobility, which prevent fertilization of Ovum., 3) Endometrial inflammatory response decrease Sperm transport & impedes ability of Sperms to, fertilize Ovum., 4) Copper Devices –, - Ionized Copper – Antifertility effect by preventing Blastocyst implantation through, enzymatic interference., 5) Levonorgestrel IVS, - It induce strong & uniform suppression of Endometrium., - Cervical mucus becomes very scanty, - Anovulation & insufficient Luteal phase activity., Time of Insertion, 1. Interval, • When insertion is made in the inter-conceptional period beyond 6 weeks following, Childbirth or Abortion., • It is preferable to insert 2 – 3 days after the menses is over., 2. Post-abortal, • Immediately following termination of pregnancy by Suction Evacuation or D & E or, following Spontaneous Abortion., 3. Post-partum, • Preferable after 6 weeks when Uterus will be involuted to near normal size., 4. Post-placental Delivery, • Vaginal as well as Cesarean Section delivery., Page 43 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur
Page 44 :
Dr. Girish Waru – Gynecology, , Method of Contraception & IUCDs, , Advantages of IUCDs, i., ii., iii., iv., , Safe & highly effective, Immediate action, Long term protection, Immediate return to Fertility after removal., , Contraindication of IUCDs, a., b., c., d., e., f., g., h., i., j., k., , Presence of pelvic infection within 3 months, Undiagnosed genital tract bleeding, Suspected pregnancy, Fibroid, Severe Dysmenorrhea, Past h/o Ectopic pregnancy, Within 6 week following C-section., STD within 3 months, Significant Immunosuppressant Patient, For Cu-T - Wilson disease, LNG –IVS – Hepatic tumor / Breast CA / Severe Arterial Disease., , Complication, A. Immediate, i., Cramp like pain, ii., Syncopal attack, iii., Partial or Complete perforation of Uterus, B. Remote, i., Pain, ii., Abnormal menstrual bleeding, iii., PID, iv., Spontaneous Expulsion, v., Perforation of Uterus., Indication for Removal of IUCDs, I., II., III., IV., V., VI., VII., VIII., IX., , Persistent excessive regular or irregular uterine bleeding, Flaring up of Salpingitis, Perforation of Uterus, IUD has come out of place, partial expulsion, Pregnancy occurring with device in situ, Woman desirous of baby, Missing treat, One year after menopause, When effective lifespan of device is over., , ………..xxx……….., , Page 44 of 44, Complied By Dr. Umesh Ramteke – CCMP-2018-19, GMC, Nagpur