Page 1 :
MSC Zoology [Final], , Dr Manish Kumar, , Date 24.05.2021, , EXCRETION AND OSMOREGULATION, KIDNEY-STRUCTURE, ANATOMY AND FUNCTION, Gross Structure, Kidneys are bean-shaped organs, about 11 cm long, 6 cm wide, 3 cm thick and weigh 150 g., They are embedded in, and held in position by, a mass of adipose tissue., Each kidney is enclosed by a thin tough fibrous connective tissue called renal capsule that, protects it from infections and injuries. Around the capsule there is a layer of fat (adipose, tissue) which is further enclosed by another layer of fibrous membrane known as renal, fascia. The bean shaped kidney have outer convex surface and inner concave surface., Location: The kidneys lie on the posterior abdominal wall, one on each side of the, vertebral column, behind the peritoneum and below the diaphragm., Position: It is situated at the level of T12-L3. The right kidney is usually slightly lower, than the left, probably because of the considerable space occupied by the liver., Anatomy of kidney, Longitudinal section of the kidney shows following parts., 1. Capsule: It is an outermost covering composed of fibrous tissue surrounding the kidney., 2. Cortex: It is a reddish-brown layer of tissue immediately below the capsule and outside, the renal It consists of renal corpuscles and convoluted tubules., 3. Medulla: It is the innermost layer, consisting of conical areas called the renal pyramids, separated by renal columns. There are 8-18 renal pyramids in each kidney. The apex of, each pyramid is called a renal papilla, and each papilla projects into a small depression,, called a minor calyx (plural calyces). Several minor calyces unite to form a major, calyx. In turn, the major calyces join to form a funnel shaped structure called renal, pelvis that collects urine and leads to ureter., , Blood supply to kidney, The renal artery enters the kidney through the hilum and then branches progressively to, form the interlobar arteries arcuate arteries, interlobular arteries, and afferent, arterioles, which lead to the glomerular capillaries. The distal ends of the capillaries of, each glomerulus combine to form the efferent arteriole, which leads to a second capillary
Page 2 :
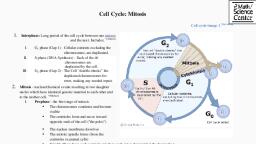
MSC Zoology [Final], , Dr Manish Kumar, , Date 24.05.2021, , network, the peritubular capillaries, that surrounds the renal tubules called vasa, recta. The blood vessels of the venous system progressively form the interlobular vein,, arcuate vein, interlobar vein, and renal vein, which leaves the kidney beside the renal, artery and ureter., Functions of Kidney:, 1. Endocrine functions: kidney is also an endocrine glands. It secretes enzymes renin, 1, 25dihydroxycholecalciferol, erythropoietin etc., Renin; It is an enzyme secreted by cells of juxtaglomerular apparatus which helps in, regulation of blood pressure., 1, 25-dihydroxycholecalciferol; it is a biological active form of vitamin D3 found in, kidney., Erythropoietin; it is essential for RBC formation, 2. Osmoregulation: Kidney regulate osmotic pressure in the body by regulating fluids and, electrolyte balance, 3. Homeostasis: also regulate PH balance, 4. Excretion: metabolic wastes of the body are excreted in the form of urea, creatinine, uric, acid etc in urine., 5. Excretion of Drugs and toxins, 6. Selective reabsorption: glucose, amino acids, water and electrolytes etc are selectively, reabsorbed in the renal tubules, 7. Erythropoiesis: helps in RBC formation, 8. Blood pressure regulation, NEPHRON-STRUCTURAL ANATOMY AND TYPES, Histologically, each kidney is composed of approximately 1 million of Uriniferous tubules, or nephron. Nephron is the structural and functional unit of the kidney.
Page 3 :
MSC Zoology [Final], , Dr Manish Kumar, , Date 24.05.2021, , Each nephron has two major portions:, 1. A Renal corpuscle (Malpighian body), 2. A Renal tubule, 1. Renal corpuscles (Malpighian body):, A renal corpuscle consists of a glomerulus surrounded by a glomerular capsule (Bowman’s, capsule)., The glomerulus is a capillary network that arises from an afferent arteriole and empties, into an efferent arteriole. The diameter of the efferent arteriole is smaller than that of the, afferent arteriole, which helps maintain a fairly high blood pressure in the glomerulus., Bowman’s capsule is double walled cup like structure and it encloses the glomerulus. The, wall of glomerulus and the Bowman’s capsule consists of a single layer of flattened, epithelial cells., Glomerular capsule consists of three layers, i) Outer parietal layer consists of squamous epithelium cells with minute pore of, 12nm diameter called fenestrations, ii) Middle basement membrane which is selectively permiable, iii) The inner visceral layer of large nucleated cell called podocytes. Podocytes, bears finger like projections known as podocels. The areas between the two, podocels is filtration slit underlying basement membrane., 2. Renal tubules:, The renal tubule continues from Bowman’s capsule and consists of the following, parts: proximal convoluted tubule (in the renal cortex), loop of Henle (in the renal, medulla), and distal convoluted tubule (in the renal cortex)., i) Proximal convoluted tubules (PCT): it is proximal part of renal tubules next to, Bowman’s capsule. It is lined with microvilli. Maximum reabsorption of water,, glucose, amino acids and electrolytes takes place here., ii) Loop of Henle: It is U shaped middle portion of renal tubules. It is composed of, ascending and descending loop. Ascending loop is thick walled and impermeable to, water while descending loop is thin walled and permeable to water. Counter current, mechanism is crucial role of loop of Henle., iii) Distal convoluted tubules (DCT): It is the distal part of renal tubules that leads, to collecting ducts. It is similar in structure and function with PCT., iv) Collecting tubules: It is not a part of nephron rather it is a part of kidney. The, distal convoluted tubules from several nephrons empty into a collecting tubule., Several collecting tubules then unite to form a papillary duct that empties urine, into a minor calyx and then into major calyx and finally into renal pelvis., Types of nephron, 1. Cortical nephron: 80% of the nephrons are short and located within the cortex., 2. Juxtamedulary nephron: 20% of nephron have long loops of Henle that extend into the, medulla.
Page 4 :
MSC Zoology [Final], , Dr Manish Kumar, , Date 24.05.2021, , PHYSIOLOGY OF URINE FORMATION, There are three stages involved in the process of urine, 1. Glomerular filtration or ultra-filtration, , formation. They are-, , 2. Selective reabsorption, 3. Tubular secretion, , Glomerular filtration, This takes place through the semipermeable walls of the glomerular capillaries and, Bowman’s capsule., , , The afferent arterioles supplying blood to glomerular capsule carries useful as well as, harmful substances. The useful substances are glucose, aminoacids, vitamins, hormones,, electrolytes, ions etc and the harmful substances are metabolic wastes such as urea, uric, acids, creatinine, ions, etc., , , , The diameter of efferent arterioles is narrower than afferent arterioles. Due to this, difference in diameter of arteries, blood leaving the glomerulus creates the pressure, known as hydrostatic pressure., , , , The glomerular hydrostatic pressure forces the blood to leaves the glomerulus resulting, in filtration of blood. A capillary hydrostatic pressure of about 7.3 kPa (55 mmHg) builds, up in the glomerulus. However this pressure is opposed by the osmotic pressure of the, blood, provided mainly by plasma proteins, about 4 kPa (30 mmHg), and by filtrate, hydrostatic pressure of about 2 kPa (15 mmHg in the glomerular capsule., The net filtration pressure is,, , , , Therefore: 55-(30 +15) = 10mmHg.
Page 5 :
MSC Zoology [Final], , Dr Manish Kumar, , Date 24.05.2021, , , , By the net filtration pressure of 10mmHg, blood is filtered in the glomerular capsule., , , , Water and other small molecules readily pass through the filtration slits but Blood cells,, plasma proteins and other large molecules are too large to filter through and therefore, remain in the capillaries., , , , The filtrate containing large amount of water, glucose, aminoacids, uric acid, urea,, electrolytes etc in the glomerular capsule is known as nephric filtrate of glomerular, filtrate., , , , The volume of filtrate formed by both kidneys each minute is called the glomerular, filtration rate (GFR). In a healthy adult the GFR is about 125 mL/min, i.e. 180 litres of, filtrate are formed each day by the two kidneys, , Selective reabsorption, As the glomerular filtrate enters the renal tubules, it flows sequentially through the successive, parts of the tubule: The proximal tubule → the loop of Henle (1) → the distal tubule (2) → the, collecting tubule → inally ,the collecting duct, before it is excreted as urine., , , As the filtrate passes to the renal tubules, useful substances including some water,, electrolytes and organic nutrients such as glucose, aminoacids, vitamins hormones etc are, selectively reabsorbed from the filtrate back into the blood in the proximal convoluted, tubule., , , , Reabsorption of some substance is passive, while some substances are actively, transported. Major portion of water is reabsorbed by Osmosis., , , , Only 60–70% of filtrate reaches the Henle loop. Much of this, especially water, sodium and, chloride, is reabsorbed in the loop, so that only 15–20% of the original filtrate reaches the, distal convoluted tubule, More electrolytes are reabsorbed here, especially sodium, so the, filtrate entering the collecting ducts is actually quite dilute., , , , The main function of the collecting ducts is to reabsorb as much water as the body needs., , , , Nutrients such as glucose, amino acids, and vitamins are reabsorbed by active transport., Positive charged ions ions are also reabsorbed by active transport while negative charged, ions are reabsorbed most often by passive transport. Water is reabsorbed by osmosis, and, small proteins are reabsorbed by pinocytosis.
Page 6 :
MSC Zoology [Final], Dr Manish Kumar, Date 24.05.2021, Mechanisms of cellular transport in the nephron, 1. Active transport “Active transport can move a solute against an electrochemical gradient and, requires energy derived from metabolism” movement of two molecules in opposite direction based on, their concentration., i. Primary active transport Transport that is coupled directly to an energy source such as ATP Sodium, potassium pump (found in basolateral membrane along renal tubules) H+-pump, ii. Secondary active transport Transport that is coupled indirectly to an energy source due to, concentration gradient of ion Na-K-2Cl co-transport glucose-sodium co-transport (SGLT) amino acidsodium co-transport H+/Na counter-transport, 2. Passive Transport “Pasive transport can move a solute down the electrochemical gradient and do not, requires energy ”, i. i. Simple diffusion (without carrier protein) Simple diffusion is basically the diffusion of substances, through a membrane without needing the help from other substances Ex-Cl, HCO3-, urea , creatinine ii., Facilitated diffusion (require carrier protein) It is the process of spontaneous passive transport (as, opposed to active transport) of molecules or ions across a biological membrane via specific, transmembrane integral proteins. Ex- Glucose and amino acids at the basalateral border (GLUT), 3. Osmosis: Water is always reabsorbed by a passive (nonactive) physical mechanism called osmosis ,, which means water diffusion from a region of low solute concentration (high water concentration) to one, of high solute concentration (low water concentration)., 4. Pinocytosis\ exocytosis : The proximal tubule, reabsorb large molecules such as proteins by, pinocytosis. In this process, the protein attaches to the brush border of the luminal membrane, then, invaginates to the interior of the cell until it is completely pinched off and a vesicle is formed containing, the protein. Once inside the cell the protein is digested into its constituent amino acids, which are, reabsorbed through the basolateral membrane into the interstitial fluid. Because pinocytosis requires, energy, it is considered a form of active transport., Tubular secretion, Tubular secretion takes place from the blood in the peritubular capillaries to the filtrate in the, renal tubules and can ensure that wastes such as creatinine or excess H+ or excess K+ ions are, actively secreted into the filtrate to be excreted., , , Excess K+ ion is secreted in the tubules and in exchange Na+ ion is reabsorbed otherwise it causes, a clinical condition called Hyperkalemia., , , , Tubular secretion of hydrogen ions (H+) is very important in maintaining normal blood pH., , , , Substances such as , e.g. drugs including penicillin and aspirin, may not be entirely filtered out of, the blood because of the short time it remains in the glomerulus. Such substances are cleared by, secretion from the peritubular capillaries into the filtrate within the convoluted tubules., , , , The tubular filtrate is finally known as urine. Human urine is usually hypertonic.
Page 7 :
MSC Zoology [Final], , Dr Manish Kumar, , Date 24.05.2021, , URINE COMPOSITION, It is pale yellow in color due presence of a pigment called urochrome., It is formed by the haemoglobin of dead RBCs., It is acidic in nature and has pH 6.1- 6.5., It has a faint aromatic odour. The bad smell is due degradation of urea into ammonia by, microbes., Daily output of urine in normal person is 1.5 1.8 litres., Chemically it consists of 95-96% water, urea 2%, uric acid 0.2%, ammonia 0.25%, and, creatine 0.5% and salts 1%., CONDUCTION OF URINE/ MICTURITION, The urine produced in the nephrons is passed into the collecting tubule which opens into, ducts of Bellini. They converge towards hilus and pass through renal pyramids, minor calices,, major calices, pelvis andureters., Ureters conduct the urine into urinary bladder by peristalsis., When urinary bladder is full of urine a reflex is initiated which cause contraction of smooth, and abdominal muscles., This drives the urine out of the body through urethra., The passing out of urine is called micturition., , COUNTER-CURRENT MECHANISM, Mammals including man and birds secrete hypertonic urine. This ability is due to presence of, counter- current mechanism. It is a main adaptation of land vertebrates for the conservation of, water. By this mechanism, the kidneys regulate the osmotic pressure of blood by regulating the, water level of blood plasma. It is called as osmoregulation. There are two counter- current, mechanisms operating inside the kidney., 1. Vasa rectae, 2.Henle’s Loop., 1. Vasa rectae
Page 8 :
MSC Zoology [Final], , Dr Manish Kumar, , Date 24.05.2021, , Inside the renal medulla, the efferent arteriole forms a peri tubular capillary network, around the tubules. It is called as vasa rectae., Only 1-2% of total renal blood flows through vasa rectae. The blood flows in opposite, directions in two limbs of vasa rectae., Blood entering the medulla in descending limb comes very close to outgoing blood in, ascending limb., When blood flows towards medulla, Na+ and Cl- diffuse in the blood from interestial fluid, but it is reversed when blood flows towards cortex., This checks the loss of Na+ and Clfrom the medulla and maintains the high concentration, of these ionsin deeper parts of medulla., 2. Henle’s Loop:, Nephric filtrate flowsin opposite directions of Henle’sloop., Large amount of Na+ is actively transported from nephric filtrate into interestial fluid, through the wall of ascending limb., It is followed by passive transport of Cl-., It increases the concentration of Na+ and Cl- in medulla. Some of Na+ and Cl- passively, diffuse into the decending limb., Na+ and Cl- from the descending limb reach ascending limb through loop of Henle. This, cyclic movement of Na+ and Cl- is called counter current mechanism., It increases Na+ and Cl- concentration in renal medulla which help to reabsorbtion of, water from glomerular filtrate., There is no water reabsorption in ascending limb because its wall is impermeable to, water. Water reabsrption mainly occurs in collecting tubules. It is aided by ADH or, vasopressin.,
Page 9 :
MSC Zoology [Final], , ROLE, OF, ADH,, OSMOREGULATION, , Dr Manish Kumar, , RENIN-ANGIOTENSIN, , Date 24.05.2021, , AND, , ALDOSTERONE, , IN, , ROLE OF RENIN-ANGIOTENSIN SYSTEM (RAS) IN OSMOREGULATION, The renin-angiotensin system (RAS) or the renin-angiotensin-aldosterone system (RAAS) is a, hormone system that regulates blood pressure and water (fluid) balance., When renal blood flow is reduced, juxtaglomerular cells in the kidneys activate their, prorenin and secrete renin directly into circulation., Plasma rennin then carries out the conversion of angiotensinogen released by the liver to, angiotensin I. Angiotensin I is subsequently converted to angiotensin IIby the, enzymeangiotensin-converting enzyme found in the lungs., Angiotensin II is a potent vaso-active peptide that causes blood vessels to constrict, resulting, in increased blood pressure. Angiotensin II also stimulates the secretion of the hormone, aldosterone from the adrenal cortex., Angiotensin-II Stimulates sodium reabsorption by the proximal convoluted tubules., Retaining Na+, raises the osmotic pressure of the blood and reduces water loss from, renal tubules, Aldosterone causes the tubules of the kidneys to increase the reabsorption of sodium and, water into the blood. This increases the volume of fluid in the body, which also increases, blood pressure., If the renin-angiotensin-aldosterone system is abnormally active, blood pressure will be too, high. There are many drugs that interrupt different steps in this system to lower blood, pressure., , , , , , , ADH (ANTI-DIURETIC HORMONE), Antidiuretic hormone (ADH) has the primary role in osmoregulation by controlling the, amount of urine formation., , , , , , ADH is also known as Vasopressin, Body maintain water and electrolytes concentration at a relatively constant level by the, mechanism of osmoregulation. Hormone are important signaling molecules that control, the regulatory process., ADH is synthesized in hypothalamus and secreted by posterior pituitary gland.
Page 10 :
MSC Zoology [Final], , Dr Manish Kumar, , Date 24.05.2021, , , , When blood become more concentrated in certain situation such as- Too little amount of, water intake, Excessive loss of water by sweating or Consumption of large amount of salt., These conditions are responsible for raised in plasma solute concentration (rise in, negative osmotic pressure) ie. Decrease in blood volume., , , , The osmo-receptor of Hypothalmus detect increase in plasma solute concentration and, signal posterior pituitary gland to release ADH., , , , ADH travel to the kidney via the blood as chemical messengers., , , , ADH regulates water reabsorption by increasing the permeability of distal convoluted, tubules and collecting ducts to water by opening water channel. Water channel are, protein, which is synthesized by Golgi complex., , , , Binding of ADH on specific cell surface receptor present in DCT and collecting ducts bring, water channel to the surface of membrane. Through water channel, water enter from, glomerular filtrate to the blood capillary, so that the volume of urine become less and, hypertonic. This phenomenon is known as Anti-diuresis., When intake of water is high, the process reversed. Release of ADH is inhibited, so the, wall of DCT and collecting duct become impermeable to water causing large volume and, hypotonic urine production. The phenomenon is known as Diuresis., Function: ADH increases the reabsorption of water by the distal tubule and collecting duct, , , , , , Feedback regulation of ADH, Hypothalamus control ADH production by negative feedback mechanism
Page 11 :
MSC Zoology [Final], , Dr Manish Kumar, , Date 24.05.2021, , 1. stimulates ADH synthesis, if osmotic concentration of extracellular fluid is high; urineconcentrated, 2. reduces ADH synthesis, if osmotic concentration of extra cellular fluid and plasma falls;, urine-dilutes, Aldosterone hormone, Aldosterone is a hormone secreted by the outer cortical layer of the adrenal gland., Angiotensin II Increases the synthesis and release of aldosterone., Aldosterone stimulate Na-K pump, so that more Na+ from the filtrate is reabsorbed by the, epithelial cells of the collecting ducts., Aldosterone also stimulate sodium absorption from gut and decrease loss of sodium from, sweat. Thus, level of Na+ increases in blood, this in turn causes more water absorption, raising the volume and blood pressure, Function: Maintain constant plasma Na+ level and also help water reabsorption