Page 1 :
REPRODUCTION IN LOWER AND, HIGHER ANIMALS, Std : XII, , Chapter no. 2, , • REPRODUCTION : It is defined as the, biological process of formation of new life, forms from the pre-existing similar life., • Also known as Procreation or Breeding, • It is important for the continuation of species., • Even though the individual organism dies after, completing its life span, its species continues, to live for a long period of time.
Page 2 :
Animals and their young ones
Page 3 :
Types of reproduction, Asexual, 1. No involvement of, gametes and their fusion., 2. Does not require meiosis., 3. Progeny is formed by a, single parent., 4. Progeny is genetically, identical to single parent., Called clones., , Sexual, 1. Involves male and female, gametes., 2. Requires meiosis to, produce gametes., 3. Both parents are involved., 4. Progeny shows variation, due to fusion of male and, female gametes (genes)
Page 4 :
Asexual reproduction by Budding., (There are two types of buds), • Internal buds, • Endogenous buds, • (During unfavourable, conditions), • Ex. Fresh water, sponges : Spongilla., , • External buds, • Exogenous buds, • (During favourable, conditions), • Ex. Budding in Hydra.
Page 7 :
BUDDING IN HYDRA
Page 8 :
SEXUAL REPRODUCTION, Important points :, , Involves the production of offspring by the formation, and fusion of gametes also called amphimixis., Gametes are formed by meiosis., The sexually reproducing animals show two main phases, in their life time., a) The earlier Juvenile phase., b) b) The later Reproductive maturity phase., , The sexually reproducing animals show various breeding, patterns. Some like goats and sheep are seasonal, breeders while humans and apes are continuous, breeders - can breed throughout the year.
Page 9 :
Human Reproduction :, Humans beings are sexually reproducing, Viviparous animals. The, process of reproduction involves various sequential steps such as :, Gametogenesis, Insemination, Internal fertilization, Zygote formation, Embryogenesis, Gestation, Parturition., Human male and female show sexual dimorphism as they can be, externally differentiated by certain specific features called secondary, sexual characters., (In males, presence of beard, moustache, hair on the chest, muscular body,, enlarged larynx (Adam’s apple) are secondary sexual characters while in females, these characters are the developed breast, broader pelvis and high pitched voice.)
Page 10 :
MALE REPRODUCTIVE SYSTEM, Labellings :, 1. Seminal vesicles, 2. Ejaculatory duct, 3. Bulbo-urethral gland, (Cowper’s gland), , 4. Urethra, 5. Epididymis, 6. Testis, 7. Urinary bladder, 8. Prostate gland, 9. Vas deferens, 10. Penis
Page 11 :
MALE, REPRODUCTIVE, SYSTEM, It consists of :, , 1. TESTIS, (Male Gonads), 2. ACCESSORY, DUCTS, 3. GLANDS, 4. EXTERNAL, GENITALIA
Page 12 :
A. TESTIS, 1. A pair of testes,, mesodermal in origin., They are located in a, pouch called scrotum., During early foetal life,, the testes develop in, abdominal cavity and, later they descend into, the scrotal sac through a, passage called inguinal, canal., Each testis is oval in, shape, 4 to 5cm long, 2 to, 3cm wide and 3cm thick.
Page 14 :
L. S. of Testis
Page 15 :
T.S. OF TESTIS, Each seminiferous tubule, is internally lined by, germinal epithelial cells, (spermatogonia) and few, large pyramidal cells called, Sertoli cells or Nurse cells, sustentacular cells., The germinal epithelial, cells undergo, gametogenesis to form, spermatozoa., Sertoli cells provide, nutrition to the developing, sperms., The Interstitial or Leydig’s, cells lie in between the, seminiferous tubules. They, secrete the hormone, testosterone (androgen).
Page 16 :
B. ACCESSORY, , DUCTS, , The accessory ducts, include :, 1. Rete testis Network of small, tubules., 2. Vasa efferentia :, 12-20 fine tubules, arising from rete, testis.
Page 17 :
3. Epididymis – It is a, long about 6mts (20 feet), and highly coiled tube., Differentiated into :, , Upper caput- Head, Middle corpus- Body, Lower cauda – Tail, The sperms undergo, maturation in epididymis., They develop the ability, to swim and fertilize in, epididymis.
Page 18 :
4. Vas deferens : Travels, upto the abdominal cavity and, loops over the ureter to open, into the urethra, , 5. ejaculatory duct :, The ejaculatory duct passes, through the prostate gland, and opens into the urethra., , 6. Urethra : Also called, urino-genital duct. In males it, is long (20 cm or 7-8 inches), and extends through the, penis. It opens to the outside, by an opening called the, urethral meatus or urethral, orifice.
Page 19 :
C. GLANDS, Seminal vesicles:, It secretes an alkaline seminal fluid, which contains fructose, fibrinogen and, prostaglandins. It contributes about 60%, of the total volume of the semen., , Prostate gland:, It releases a milky white and slightly, acidic prostatic fluid into the urethra. It, forms about 30% of volume of semen. It, contains citric acid, acid phosphatase, and various other enzymes., , Cowper’s gland /, Bulbourethral gland:, These glands secrete an alkaline,, viscous, mucous like fluid which acts as, a lubricant during copulation.
Page 20 :
SEMEN (Seminal plasma), 1. It is the viscous, alkaline and milky fluid, (pH 7.2 to 7.7)., 2. Normally 2.5 to 4.0 ml of semen is given, out during a single ejaculation., 3. It contains about 400 million sperms., 4. It contains secretion of the epididymis and, the accessory glands.
Page 21 :
D. EXTERNAL GENITALIA, 1. PENIS :, It is the male, copulatory organ. It is, cylindrical and, muscular made up of, bundles of erectile, tissuecorpora cavernosa, and, corpus spongiousm., The swollen tip of the, penis is called glans, penis. It is covered by, a loose fold of skin, called foreskin or, prepuce.
Page 22 :
2. SCROTUM :, 1. Loose pouch of pigmented skin., 2. The foetal testis remain attached, to the scrotum by a muscular band, called gubernaculum., 3. The testes remain suspended in, scrotum by a spermatic chord., 5. During early foetal life, the testes, develop in abdominal cavity and, later they descend into the scrotal, sac through a passage called, inguinal canal., 6. Failure of testis to descend into, scrotum is called cryptorchidism. It, results in the sterility., 7.The temperature in the testis, remain 2-3 degree Celsius lower, than the normal body temperature,, necessary for spermatogenesis.
Page 25 :
FEMALE REPRODUCTIVE SYSTEM, The female reproductive system consist, of the following parts :, , 1. A pair of ovaries, (Female gonads), 2. A pair of oviducts, , 3. Uterus, 4. Vagina, 5. External genitalia (vulva), 6. A pair of vestibular glands, 7. A pair of mammary glands
Page 26 :
1. OVARY, 1. Ovary : Primary female sex, organ., 2. Solid, oval or almond, shaped., 3. Located in the upper lateral, part of the pelvis., 4. The broad ligament holds, the ovary, oviduct and the, uterus to the dorsal body, wall., 5. The ovarian ligament, attaches ovary to the uterus., 6. The ovary produces the, , ovum and five hormones, viz, estrogen, progesteron,, relaxin, activin and inhibin.
Page 27 :
DEVELOPMENT OF, OVARY :, During early embryonic, development, cells, from the dorsal, endoderm of the yolk, sac migrate along the, hindgut to the gonadal, ridge. These primordial, germ cells (germinal, epithelium) multiply by, mitosis and once they, have reached the, gonadal ridge they are, called oogonia (diploid, stem cells of the, ovary).
Page 28 :
The process of oogenesis starts much before the birth of the, female baby and by the end of twelve weeks the ovary is fully, formed. It has more than two million primordial follicles in it.
Page 29 :
STRUCTURE OF OVARY, Each ovary is a compact structure covered on the outside by Tunica Albuginea and is, internally differentiated into an outer part called cortex and a central part called medulla ., , Cortex : Covered, externally by a layer of, germinal epithelium., The cortex is more, compact and granular. It, shows large number of, Ovarian Follicles in, different stages of, development ., Medulla : The loose, connective tissue of the, medulla called stroma, has blood vessels,, lymph vessels, and, nerve fibres.
Page 30 :
T.S. of Ovary
Page 31 :
Formation of Primordial Follicles :, During Embryonic development some cells of germinal epithelium become large, sized and multiply mitotically to from a group of cells called egg mother cells or, oogonia. The oogonia now project into the stroma of the ovary as a cord, the egg, tube of Pfluger which later becomes a round mass, the egg nest., The cell at the top in the egg nest grows and becomes the, primary oocyte (future ovum). Other oogonia in the nest, form the follicular epithelium around the primary oocyte to, protect and nourish it. The structure thus formed is called, Primordial Follicle. So each primordial follicle has, at its, center a large primary oocyte (2n) surrounded by a single, layer of flat follicular cells., About two million primordial follicles in the foetal ovary., About one million remain at birth and only about 40,000, remain at the time of puberty., The large scale destruction of the primordial follicles during, growth is called Atresia., The development of the primordial follicles into mature or, Graafian follicles restarts with the onset of puberty., , Primordial follicle
Page 32 :
Formation of Graafian, Follicle and Ovulation, Each primary follicle has, multi-layered cuboidal, follicular cells. The stroma, cells add theca over the, follicle to form secondary, follicle., The secondary follicle grows, into the Graafian follicle by, addition of more follicular, cells., Release of Graafian follicle is, called ovulation., Temporary endocrine gland, called corpus luteum is, formed., No fertilization - corpus, luteum degenerates into a, white scar called corpus, albicans.
Page 35 :
STAGES IN DEVELOPMENT OF OVUM, Germinal epithelium, , Oogonia, Primary oocyte, Primordial follicle, Primary follicle, Secondary follicle, Tertiary follicle, , Graafian follicle, , OVUM
Page 36 :
2. OVIDUCT/FALLOPIAN, TUBE/UTERINE TUBE, A pair of muscular ducts., Internally lined by ciliated, epithelium. It can be divided into, three regions :, a. Infundibulum : The proximal, funnel like part lying close to the, ovary with an opening called, ostium surrounded by fimbriae., b. Ampulla : Middle, long and, straight part of the oviduct., Fertilization of the ovum takes, place in this region., c. Isthmus / Cornua : The distal, narrow part of the duct opening, into the uterus.
Page 37 :
3. UTERUS, (WOMB), It is a hollow, muscular,, pear shaped organ,, located above and, behind the urinary, bladder. It is divided, into three regions :, , a. Fundus., b. Body., c. Cervix., Internally the uterus is, made up of 3 layers :, , 1. Perimetrium, 2. Myometrium., 3. Endometrium
Page 38 :
4. VAGINA, Tubular, elastic, muscular canal, with a soft, flexible lining that, provides lubrication and, sensation, It is the female copulatory, organ, 7 to 9 cm in length. It lies, between the cervix and the, vestibule., The vaginal wall has an inner, mucosal lining, the middle, muscular layer and an outer, adventitia layer., The opening of the vagina into, the vestibule is called vaginal, orifice which is covered partially, by a fold of mucous membrane, called hymen., The vagina acts as a passage for, menstrual flow as well as birth, canal during parturition.
Page 39 :
5. EXTERNAL, GENITALIA, These include parts external to the vagina and, are collectively called ‘vulva’ (covering or, wrapping), or pudendum. They include the, following parts :, a. Vestibule - It is a median vertical depression, of vulva enclosing the urethral and vaginal, opening., b. Labia minora - These are another pair of, thin folds inner to the labia majora, c. Clitoris - A small conical and sensitive, projection at the antirior end of labia minora., It has a pair of erectile tissue – The corpora, cavernosa and is homologous to the penis., d. Labia majora - These are a pair a fleshy, folds of skin forming the boundary of vulva., They are homologous to the scrotum, e. Mons pubis - It is a fleshy elevation above, the labia majora
Page 40 :
6. ACCESSARY GLANDS / VESTIBULAR GLANDS /, BARTHOLIN’S GLANDS, It is a pair of glands homologous to the Bulbourethral or Cowper’s, glands of the male. They open into the vestibule and release, lubricating fluid.
Page 41 :
7. MAMMARY GLANDS, ● Modified sweat glands., ● Each mammary gland contains, fatty connective tissue, glandular, tissue and numerous lactiferous, ducts., ● The glandular tissue forms 15-20, mammary lobes., ● Each lobe has many alveolar glands, and lactiferous duct., ● These ducts converge towards the, nipple located near the tip of the, breast., ● Nipple is surrounded by areola., ● Accessory reproductive organs for, production and release of milk., ● Specifically, only women who have, given birth have functioning, mammary glands.
Page 42 :
Alveolar glands secrete milk which is stored in the lumen of alveoli., The alveoli open into mammary tubules. The tubules of each lobe join, to form a mammary duct. Many mammary ducts join to form a wider, mammary ampulla, which is connected to lactiferous duct., Lactiferous ducts are known by many names, including milk ducts,, mammary ducts, and galactophores. These converge towards the, nipple.
Page 44 :
PUBERTY/SEXUAL MATURITY IN MALES, Puberty is the age at, which the reproductive, system becomes, functional., Sex organs begin to, produce gametes and, sex hormones., In males the onset of, puberty occurs at age, 12-15 years., Under the influence of, testosterone, the, secondary sexual, characters appear., Thereafter it remains, functional throughout, the life.
Page 45 :
PUBERTY/SEXUAL MATURITY IN FEMALES, Functional reproductive system., First menstrual cycle begins also called, Menarche (at 10- 14 years)., These are the cyclic changes that the, mature females show in their, reproductive system., These cycles continue only upto, Menopause(45-50 years)., Menarche to Menopause is thus the, Reproductive age of female which is, approximately 32 years (age 13 to 45)., In this time the female will be, producing a maximum of about 416, eggs (32 ×13 = 416 eggs)., The female is unable to bear children, (by natural method) after menopause., Menarche, menstrual cycles and menopause are controlled by gonadotropic hormones.
Page 46 :
MENSTRUAL CYCLE (Ovarian cycle), Characteristic feature of primates including human., It involves a series of cyclic changes in the ovary and the female, reproductive tract, mainly in the uterus., These changes are influenced by gonadotropins and the ovarian, hormones., The cycles are repeated with a periodicity of approximately 28 days., The middle of each cycle releases an egg (Ovulation)., This egg is produced alternately from any one of the two ovaries in, each cycle., The cycle is divided into four phases:, , 1., 2., 3., 4., , MENSTRUAL PHASE, PROLIFERATIVE PHASE, OVULATORY PHASE, SECRETORY PHASE
Page 48 :
1. Menstrual phase :, The first phase(average of 5 days), where menses or loss of blood (45100ml) takes place., Prostaglandins are released due to, decreased levels of progesteron and, estrogen., Due to this blood, tissue fluid, mucus,, endometrial lining and the unfertilized, oocyte is discharged through vagina., along with the menstruum. It is thus, called ‘funeral of unfertilized egg’., Endometrium thickness 1mm, During these five days, many, primordial follicles develop into, primary and few of them into, secondary follicles under the effect of, FSH., However this blood does not clot due to, presence of fibrinolysin.
Page 49 :
2. Proliferative phase :, It is the Second phase of, Menstrual cycle, generally from, 5th to 13th day of the cycle., A few secondary follicles begin, development but usually one of, them develops into a Graffian, follicle ., Oestrogen is secreted., The other secondary follicles, degenerate (Atresia)., Proliferation is influenced by GnRH, which stimulates release of FSH., Endometrium begins to regenerate, under the effect of gradually, increasing quantity of estrogens., Regeneration also involves, formation of endothelial cells,, endometrial or uterine glands and, network of blood vessels., Endometrium thickness :3-5 mm.
Page 50 :
3. Ovulatory phase :, Shortest phase of menstrual, cycle., It involves rupturing of the, mature graffian follicle and, release of ovum (secondary, oocyte)., Usually on 14th day of, menstrual cycle., Rapid secretion of LH by, positive feedback mechanism, causes the mature follicle to, rupture., Ovulation may be, accompanied by mild or, severe pains in lower, abdomen., Endometrium continues to, grow.
Page 51 :
4. Secretory phase :, Longest phase lasting 14 days., After ovulation, remaining tissue of, graffian follicle transforms into corpus, luteum under the effect of LH., Corpus luteum begins to secrete, progesterone and estrogens., Under the influence of these hormones,, the endometrial glands grow, become, coiled and start uterine secretions., Endometrium is 8-10 mm thick and, more vascularized., If no fertilization, corpus luteum forms, corpus albicans., Inhibin stops secretion of FSH., If ovum is fertilized, and embryo is, implanted-- secretion of (hCG), so, corpus luteum persists., Presence of hCG in maternal blood and, urine is an indicator of pregnancy., If no fertilization, next menstrual cycle, begins.
Page 52 :
GAMETOGENESIS:, The gametogenesis is the process of formation of gametes in sexually, reproducing animals., Spermatogenesis – Sperms, Oogenesis – Ovum, The gametes are formed by meiosis in which the number of chromosomes are, reduced from Diploid to Haploid, Gametes are formed from primordial germ cells of gonads.
Page 53 :
SPERMATOGENESIS:, Formation of the male gamete (sperm)., At Puberty, the hypothalamus begins secretion of (GnRH)., GnRH initiates secretion of (FSH) which induces spermatogenesis., , Spermatogenesis involves three, phases :, I. Multiplication phase: The, primordial germ cells (2n) of, seminiferous tubules undergo, repeated mitotic divisions to, produce large number of, spermatogonia (2n). Each, spermatogonium is diploid with 46, chromsomes., , II. Growth phase:, Some of the spermatogonia stop, dividing and grow in size to develop, into primary spermatocytes (2n) due, to accumulation of food.
Page 54 :
III. Maturation phase:, It involves meiotic division., The primary, , spermatocyte (2n), undergoes the first meiotic, division (meiosis I) forming, two haploid cells called, , secondary, spermatocytes (n)., The secondary, spermatocyte undergoes, second meiotic division, (meiosis II) to produce four, haploid spermatids. The, spermatid is non-motile and, non-functional., It gets transformed into a, functional spermatozoa by, the process called, spermiogenesis.
Page 55 :
SPERMIOGENESIS., 1. The sperm heads remain attached to the sertoli cells and their tails hanging in, the lumen of seminiferous tubule., 2. Length of spermatid increases., 3. Centrioles are rearranged as primary and distal centrioles., 4. Mitochondria become spirally coiled and acrosome is formed from golgi complex.
Page 56 :
STRUCTURE OF SPERM :, It is a motile, microscopic elongated cell. It is, divisible into three parts :, Head: Oval in shape and contains haploid, nucleus. Acrosome is present above the, nucleus. Acrosome contains enzymes that help, the sperm to penetrate the ovum during, fertilisation., Neck: It is a very short region having two, centrioles i.e. proximal centriole and distal, centriole., Middle piece: It has an axial filament, surrounded by 10-14 spiral turns of, mitochondria (nebenkern). It provides energy, to the sperm., Tail: It is a long, slender and tapering part, containing cytoplasm and fine thread- axial, filament. The axial filament arises from the, distal centriole.
Page 58 :
OOGENESIS:, Formation of the haploid female gamete (egg or ovum)., It involves the process of meiosis., This process can be divided into three stages :, , I. Multiplication phase: In this stage, the primary, germinal cells (2n) of ovary undergo repeated, mitotic division to form millions of oogonium(2n)., This process is completed in the embryonic stage., II. Growth phase: Some of the oogonia stop division, and begin to increase in size and form the primary, oocytes (2n). Cellular organelles like ER, golgi, apparatus and mitochondria increase in number.
Page 60 :
III. Maturation phase:, The primary oocytes (2n) which was arrested at Prophase I, enter the, maturation phase which includes meiotic divisions (Meiosis I and Meiosis II), and forms 2 haploid daughter cells., This division is peculiar in females because both the haploid daughter cells, have unequal division of cytoplasm, one is a large cell called secondary, oocyte (n) and another is a small cell called 1st polar body (n)., Normally the 1st polar body does not enter meiosis II. The secondary oocyte, (n) proceeds meiosis II, It’s division is further arrested at metaphase II., The restart and completion of meiosis II (arrested at Metaphase II) will, happen only with entry of the sperm., This last phase is usually completed in the ampulla of the fallopian tube at, the time of fertilization., In this division also, the two unequal daughter cells are formed- the large cell, is ovum (n) and the small cell is 2nd polar body (n). The ovum (n) so formed, functions as the female gamete and is ready for fertilization., *(Completion of meiosis II and completion of fertilization go hand in hand. If the, secondary oocyte does not receive the sperm / spermatozoa, it is shed off along, with menstrum).
Page 64 :
Structure of Secondary oocyte:, Ovulated egg is actually the secondary oocyte., It is non-cleidoic and micro-lecithal., It is approximately 0.1mm (100 microns) in size., It is rounded, non motile haploid female gamete., The nucleus of the egg appears large and is called, germinal vesicle., Typical nucleus or pronucleus is formed at the time, of fertilization., The cytoplasm of egg is also called ooplasm. It is, devoid of centrioles., The egg is surrounded by various coverings
Page 65 :
The egg is surrounded by various coverings, The egg membrane is called Vitelline, membrane., It secretes a non-cellular membrane,, Zona pellucida on its outside., Adhering to the outer surface of zona, pellucida are several radially, elongated cells forming the Corona, radiata., They are firmly held to the zona, pellucida and to each other by, hyaluronic acid., Between the vitelline membrane and, the zona pellucida is a fluid filled, perivitelline space. The first polar, body lies in this space., The egg shows polarity. The side having germinal vesicle and first polar body is, called animal pole while the side opposite to it is called vegetal pole.
Page 66 :
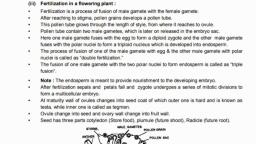
FERTILIZATION, (SYNGAMY), , , , , , , Fertilization is the fusion of, haploid male and female, gametes resulting in the, formation of a diploid, zygote (2n)., In humans the process of, fertilization is internal and, it usually takes place in the, ampulla of the fallopian /, uterine tube., The fertilized egg or zygote, will develop into an embryo, and this process occurs, within the uterus.
Page 67 :
Mechanism of fertilization, Sperms are released during ejaculation along with semen., Newly ejaculated sperm is incapable of fertilizing the ovum., Sperms can remain viable for 24-48 hrs (Ovum about 24 hrs)
Page 68 :
The mechanism of fertilization takes place as follows :, a. Movement of sperm towards egg :, After entering the vagina, about 50% sperms are destroyed., Remaining sperms undergo capacitation (5-6 hours), Capacitation :, Sperms aquire the ability to fertilize., Acrosome membrane becomes thin,, Ca++ enters the sperm and their tails, show rapid whiplash movements., The prostaglandins activate the sperms., The vestibular secretions (female) also, enhance sperms motility., Sperms become extra active and move, upwards towards the oviducts., After capacitation, the sperms may, reach ampulla within 5 minutes.
Page 69 :
b. Entry of sperm into the egg :, Sperms are attracted toward eggs of their species by chemotaxis., Though many sperms reach the, ampulla but only a single sperm, fertilizes the ovum., A sperm after reaching the ovum, comes to lie against it., Its acrosome releases lysins :, hyaluronidase and corona, penetrating enzymes., They separate and dissolve the cells, of corona radiata, so the sperm head, passes through the zona pellucida of, egg., The zona pellucida has fertilizin that, binds to antifertilizin of sperm., Fertilizin-antifertilizin interaction is, species specific., Fertilizin-antifertilizin reaction is also, called compatibility reaction.
Page 70 :
Acrosome reaction :, As the sperm head touches the zona pellucida, its acrosome, releases acrosin(zona lysin) which acts on the zona pellucida at, the point of contact., This causes egg reaction - A small fertilization cone / cone of, reception is formed on the egg membrane., The sperm head comes in contact with this cone. Plasma, membrane of both the cells dissolve at the point of contact., Only the sperm nucleus and the centrioles enter the egg., As the sperm head touches the vitelline membrane, a cortical, reaction gets activated changing the vitelline membrane into a, fertilization membrane by deactivating the sperm receptors of, zona pellucida., A distinct perivitelline space is created around the fertilization, membrane. This prevents polyspermy.
Page 73 :
c. Activation of ovum :, The ovum before fertilization was at metaphase II stage., With contact of sperm head to the vitelline membrane of egg, it, gets activated to resume and complete its meiosis II., Second polar body is formed., The germinal vesicle organizes into female pronucleus., At this stage, it is the true ovum or egg.
Page 75 :
Fusion of egg and sperm :, 1. The coverings of male and female, pronuclei degenerate allowing the, chromosomal pairing., 2. This results in the formation of a, synkaryon by the process called, syngamy., 3. Syngamy is the fusion of two gametes in, fertilization., 4. It involves both plasmogamy and, karyogamy., 5. This results in the formation of ZYGOTE., 6. The proximal centriole recieved from, the sperm helps in formation of the, synkaryon spindle and cleavage of cell, into two blastomeres.
Page 77 :
SIGNIFICANCE OF FERTILIZATION :, Secondary oocyte completes the process of oogenesis, and is transformed into a mature ovum (n)., The diploid chromosome number is restored in the, zygote by the process of syngamy., The ovum lacks the centrioles necessary for further, divisions, are received from the sperm during, fertilization., Fertilization involves fusion of male and female, gametes from the two parents. It results in variations, which are significant to evolution., Sex of the offspring is determined.
Page 78 :
EMBRYONIC DEVELOPMENT :, The zygote formed as a result of syngamy is activated to divide., CLEAVAGE : It is the process of early mitotic division of the zygote, into a hollow multicellular blastula. The cells formed by cleavage are, called blastomeres., There is no growth phase between the cleavages., Size of blastomeres reduces with every successive cleavage., So the metabolic rate increases., Subsequent cleavages are thus faster than earlier one., So there is rapid replication of DNA and high consumption of oxygen., Process of cleavage :, In human, cleavage is holoblastic i.e. the whole zygote gets divided., The cleavage planes may be longitudinal (meridional) and equatorial, (horizontal). It is radial and indeterminate i.e. fate of each blastomere, is not predetermined.
Page 79 :
The 1st cleavage in the zygote is meridional and occurs, at about 30 hours after fertilization. It divides the, zygote longitudinaly into two uneven blastomeres, one, slightly larger than the other., The 2nd cleavage is also longitudinal and occurs after, 30 hours of 1st cleavage., The 3rd cleavage is horizontal. After 3rd cleavage the, embryo is in 8-cell stage.
Page 80 :
The young embryo is gradually being pushed towards the uterus., By the end of 4th day after fertilization, embryo is a solid ball of, 16-32 cells externally looking like mulberry. This stage is thus, called morula., The morula shows two types of cells : smaller, clearer cells, towards the outer side and inner cell mass of larger cells., Till the formation of morula the zona pellucida is retained and, thus, there is no change in the overall size from zygote to morula., The morula reaches the isthmus and gains entry into the uterus, by the end of day 4.
Page 81 :
BLASTULATION, It is the formation of hollow and multicellular, blastocyst., The outer layer of cells in the morula form the layer, called trophoblast., Trophoblast cells begin to absorb the glycogen rich, uterine milk. The blastocyst doubles in size., As more fluid enters, the blastocyst cavity is formed., The inner larger cells form inner cell mass or, embryoblast. These remain attached to the, trophoblasts on one side., The trophoblast cells in contact with the embryonal, knob are called cells of Rauber., At this stage, the blastocyst shows polarity showing, embryonal end and the abembryonal end., By the end of the 7th day the blastocyst is fully, formed. It is now ready for implantation and, gastrulation within the uterus, hence zona pellucida, now ruptures.
Page 83 :
IMPLANTATION :, This process usually begins on day 7 after fertilization and by end of day 10, the, embryo is completely buried inside the endometrium., Embryo usually implants in the fundus of the uterus., The embryo attaches itself by its embryonic pole, close to the endometrium., The trophoblast cells of the animal pole stick to the uterine wall. Rapid division of, the trophoblast cells lying against the embryonal knob takes place., It results in the formation of two distinct layers, outer- syncytio-trophoblast and, inner- cyto-trophoblast., , Syncytio-trophoblast, gives out processes which, extensively invade the, endometrium., The lytic enzymes, secreted by the, trophoblasts, rupture the, endometrial cells thereby, making a burrow, into, which the embryo begins, to get implanted.
Page 85 :
GASTRULATION :, Formation of ‘gastrula’ from the blastocyst., Rate of cleavage or divisions slows down., Gastrulation begins in the embryoblast cells on, about 8th day after fertilization., , Two important events take place actively :, a. Differentiation of blastomeres :, This process results in the formation of three, germinal layers i.e. ectoderm, mesoderm and, endoderm from the cells of the embryoblast., b. Morphogenetic movements :, These are different types of movements to reach their, definite place in the embryo.
Page 86 :
Cell on the free end of inner cell mass called hypoblasts, (primitive endoderm) become flatend, start dividing and, grows downward towards the blastocoel., This layer called endoderm is the first to differentiate. It, grows within the blastocoel and forms a sac called Yolk sac., The remaining cell of the inner cell mass, in contact with, cells of Rauber are called epiblasts (primary ectoderm)., After formation of endoderm the second layer to be, differentiated is the ectoderm. Both layers form a flat,, bilaminar embryonal disc., Cells of epiblast divide and re-divide and move in such a, way that they enclose a cavity called the amiotic cavity., The floor of this cavity has the embryonal disc.
Page 87 :
The pyramidal cells of the disc towards the amniotic, cavity form the embryonal ectoderm., The roof of amniotic cavity is lined by amniogenic, cells. Later, these cells divide and re-divide to form, the amnion., As a result of all these changes, the bilaminar, embryonic disc is positioned in between amniotic, cavity and Yolk sac.
Page 89 :
Actual gastrulation occurs about 15 days after fertilization, in which, the bilaminar embryonic disc is transformed into trilaminar, embryonic disc., This transformation occurs by division, rearrangement and, migration of cells of epiblast., It begins with formation of primitive streak and a shallow groove, on the surface called primitive groove.
Page 90 :
This streak progresses from posterior to anterior end of embryo., , From site of a primitive streak, a third layer of cells called, mesoderm extends between ectoderm and endoderm., Anterior end of primitive groove communicates with yolk, sac by an aperture called blastopore (future anus)., The embryonal disc, now has, differentiated into, three layers, ectoderm, mesoderm, and endoderm., The further process, after gastrulation is, called organogenesis.
Page 92 :
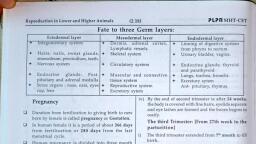
Fate of germinal layers
Page 93 :
PREGNANCY :, (GESTATION), The condition of carrying one or, more embryos in the uterus. It is, the period between fertilization, of the egg, upto parturition., The average period of, pregnancy in human lasts for, 266 days (38weeks) from, fertilization or 280 days, (40weeks) (266+14) counted, from LMC., This pregnancy period of, approximately nine months is, divided into three trimesters of, three months each.
Page 94 :
FIRST TRIMESTER, (from fertilization to 12th week), The embryo receives nutrients in the first 2-4 weeks directly from, the endometrium., It is the main period of organogenesis and by the end of eight, weeks, the major structures found in the adult are formed in the, embryo in a rudimentary form., The embryo is now called foetus. It is about 3cm long and looks, like a tiny human being., Foetus can swallow and open and close its mouth and fists., CNS is fully formed, working of excretory and circulatory systems, begins. Movements of foetus begin but mother can not feel it., Heart beat can be heard from 6th week., Progesterone level becomes high and menstrual cycle is, suspended till the end of pregnancy., At the end of first trimester foetus is about 7-10 cm long.
Page 96 :
The mother’s body, also undergoes, rapid changes., High levels of, progesterone, initiate changes in, her reproductive, system., The maternal part, of placenta grows., The uterus becomes, larger., In this period, the, mother experiences, ‘morning sickness’.
Page 97 :
SECOND TRIMESTER, (from 13th to 26th week), Rapid growth of foetus. It grows to about 30 cms. Development of, brain begins. The baby reaches half the size of a newborn., The uterus grows enough for the pregnancy to become obvious., The placenta completely takes over the production of, progesterone which maintains the pregnancy., Ultrasound at 18-20, weeks can predict the, estimated due date of, delivery., Baby’s movements can be, easily felt by the mother., Head has hair, eyebrows, and eyelashes appear,, pinnae are distinct.
Page 98 :
THIRD (FINAL), TRIMESTER, (from 27th week till the parturition), , The foetus grows to about 3-4, kg in weight and 50 cms in, length. Eyes are open. There is, gain in body weight., As the foetus grows, the uterus, expands around it., The mother’s abdominal organs, become compressed and, displaced., At the end of third trimester the, foetus becomes fully developed, and is ready for parturition.
Page 100 :
PLACENTA, Flattened, discoidal organ in the, uterus of a pregnant woman., Temporary, structural and, functional connection between, foetal and maternal circulation., Facilitates the supply of oxygen, and nutrients and also for removal, of carbon dioxide and excretory, wastes produced by the foetus., Also acts as an endocrine tissue, and produces hormones like hCG,, progesterone and estrogen., These hormones are required for, foetal growth and maintenance of, pregnancy.
Page 102 :
The placenta is attached to the, wall of the uterus and to the, baby’s umbilical cord., Placenta is the only organ, which, is formed of tissues from two, different individuals- the mother, and the foetus., Part of the placenta contributed, by the foetus is called the foetal, placenta and it is the chorionic, villi., The other part which is rich in, blood supply shared by the, mother is a part of uterine wall,, termed as maternal placenta., So human placenta is called, , haemochorial.
Page 103 :
The umbilical cord, is formed of three, blood vessels., Of these three, blood vessels, two, are small arteries, which carry blood, towards the, placenta and one, is a large vein, which returns, blood to the, foetus.
Page 104 :
The umbilical VEIN (veins flow blood to, the baby's heart) therefore it carries, oxygenated blood., The umbilical ARTERY (arteries flow, blood away from the heart) returns the, blood that has off-loaded oxygen to the, baby/foetus and so is deoxygenated, in, order to pick up more oxygen again, from the placenta.
Page 105 :
PARTURITION, Humans are viviparous., Parturition is the process of giving birth to a baby., The events involved in parturition like uterine and abdominal, contractions, dilation of cervix and passage of baby are collectively, called labour. Labour is accompanied by labour pains., Parturition is controlled by complex neuroendocrine mechanism., Signals arising from the fully formed foetus and placenta cause mild, uterine contractions, It is accompanied by rise in estrogen - progesterone ratio, increase in, oxytocin receptors in uterine muscles., The fully developed foetus gives signals for the uterine contractions by, secreting Adrenocorticotropic Hormone (ACTH) from pituitary and, corticosteroids from adrenal gland., This triggers release of oxytocin from mother’s pituitary gland, which, acts on uterine muscles of mother and causes vigorous uterine, contractions. This leads to expulsion of the baby from the uterus.
Page 106 :
It involves the following three steps :, 1. Dilation stage :, Uterine contractions begin from top, forcing the, baby towards the cervix., Contractions are accompanied by pain caused by, compression of blood vessels., Oxytocin induced uterine contractions become, stronger and stronger due to stimulatory reflex., As the baby is pushed down in the uterus, its head, comes to lie against cervix. Cervix gets dilated. The, vagina also dilates., This stage of labour can normally last upto few, hours. It ends in rupturing of amniotic membrane of, foetus.
Page 108 :
2. Expulsion, , stage :, , The uterine and abdominal contractions become, stronger. In normal delivery, the foetus passes out, through cervix and vagina with head in forward, direction., It takes 20 to 60 min. The umbilical cord is tied and, cut off close to the baby’s navel., 3. After, , birth :, , After the delivery of the baby the placenta separates, from the uterus and is expelled out as “after birth”,, due to severe contractions of the uterus., This process happens within 10 to 45 minutes of, delivery.
Page 109 :
LACTATION, The production of milk by the mammary glands is, called lactation., Prolactin is responsible for production of milk., Lactation helps the mother in feeding the new born, baby., , Colostrum: It is the sticky and yellowish fluid secreted, by the mammary glands soon after child birth. It, contains proteins, lactose and mother’s antibodies., The fat content in colostrum is low. The antibodies, help in developing resistance for the new born baby, as its own immune response is not fully developed.
Page 110 :
REPRODUCTIVE HEALTH, A society with people having physically and, functionally normal reproductive organs and normal, emotional and behavioural interactions amongst them, in all sex-related aspects is called reproductively, healthy society., To attain total reproductive health is an important, social goal of India., India was amongst the first few countries in the world, to initiate action plans and programmes to improve the, reproductive health covering wide areas related to, reproduction., These programs are currently in operation under the, Reproductive and Child Health Care (RCH) programmes.
Page 111 :
GOALS OF RCH PROGRAMMES, 1.To create awareness among people about, various aspects related to reproduction., 2.To provide facilities to people to understand, and build up reproductive health., 3.To provide support for building up a, reproductively healthy society., 4.To bring about a change mainly in three, critical health indicators i.e. reducing total, infertility rate, infant mortality rate and, maternal mortality rate.
Page 112 :
The goals of RCH can be achieved by the following ways:, 1. By introduction of sex education in schools., 2. With the help of audio- visual and the print Media., 3. By educating the younger generation about birth control, measures, pre-natal care of pregnant woman and post-natal, care of the mother and child, importance of breast feeding., 4. By developing awareness about problems arising due to, uncontrolled population growth, social evils like sex abuse, and sex related crimes and take up steps to prevent them., 5. By creating awareness about statutory ban on, amniocentesis for sex determination., 6. By creating awareness about child immunization, programmes., 7. By educating couples to reduce mortality rate of new borns, and maternal mortality rate.
Page 113 :
BIRTH CONTROL, The birth control measures which deliberately prevent fertilization are referred, to as contraceptives. They help to prevent unwanted pregnancies., An ideal contraceptive should be easily available, user friendly, effective and with, no or least side effects., Contraceptive methods are of two main types: temporary and permanent., A. Temporary methods : These are of following types :, , 1. Natural method/ Safe period / Rhythm method, 2. Coitus Interruptus or withdrawal, 3. Lactational amenorrhea, 4. Chemical means (spermicides), 5. Mechanical means / Barrier methods, a. Condom, b. Diaphragm, cervical caps and vaults, c. Intra-uterine devices (IUDs), , 6. Physiological (Oral) Devices, 7. Other contraceptives, B. Permanent Method
Page 114 :
1. Natural method/ Safe period / Rhythm method :, The principle of avoiding chances of fertilization is used., A week before and after menstrual bleeding is considered, the safe period for sexual intercourse., This idea is based on the fact that ovulation occurs on the, 14th day of menstrual cycle., Its drawback : high rate of failure., , 2. Coitus Interruptus or withdrawal :, The male partner withdraws his penis from the vagina just, before ejaculation, so as to avoid insemination., Drawbacks : as the pre-ejaculation fluid may contain, sperms, this can cause fertilization.
Page 115 :
3. Lactational amenorrhea (absence of menstruation) :, This method is based on the fact that ovulation does not, occur during the period of intense lactation following, parturition., When the mother breastfeeds the child fully, chances of, conception are almost negligible., This method also has high chances of failure., , 4. Chemical means (spermicides):, Before intercourse, if chemicals like foam, tablets, jellies,, and creams are introduced into the vagina, they stick to, the mucous membrane, immobilize and kill the sperms., It may cause allergic reaction., This method also has chances of failure.
Page 116 :
5. Mechanical means / Barrier methods:, With the help of barriers the ovum and sperm are, prevented from physically meeting., These mechanical barriers are of three types :, i) CONDOM, It is a thin rubber sheath, used to cover the, penis during copulation., It prevents the entry of ejaculated semen into, the vagina., This can prevent conception., It is a simple and effective method and has no, side effects., “Nirodh” is the most widely used contraceptive, by males., Condom is also a safeguard against STDs and, AIDS.
Page 117 :
II. DIAPHRAGM, CERVICAL, CAPS AND VAULTS, These devices used by, the female are made up, of rubber., They prevent, conception by blocking, the entry of sperms, through the cervix., The device is inserted, into the female, reproductive tract to, cover the cervix during, copulation.
Page 118 :
iii) INTRA-UTERINE DEVICES, (IUDs), These clinical devices are plastic, or metal objects., A doctor or trained nurse places, the IUDs into the uterus., These devices include :, a. Lippes loop, b. copper releasing IUDs (Cu-T,, Cu7, multiload 375), c. Hormone releasing IUDs, (LNG-20, progestasert).
Page 119 :
Lippes loop is a plastic double “s” loop., It attracts the macrophages in the uterine, cavity. Macrophages increase, phagocytosis of sperms and acts as a, contraceptive., Copper releasing IUDs suppress sperm, motility and the fertilizing capacity of, sperms., The hormone releasing IUDs make the, uterus unsuitable for implantation and, cervix hostile to the sperms., It delays pregnancy for longer period., The spontaneous expulsion, occasional, haemorrhage and chances of infection are the, drawbacks of IUDs.
Page 120 :
6. PHYSIOLOGICAL (ORAL) DEVICES, They are used in the form of tablets, and hence are called pills. It is an oral, contraceptive, used by the female., The pill contains progesteron and, estrogen. They inhibit ovulation, so, no eggs are released from the ovary, and thus conception cannot occur., They also alter the quality of cervical, mucus to prevent the entry of sperms., The pills have side effects such as, nausea, weight gain, tenderness of, breast and slight blood loss between, menstrual periods., The pill “Saheli” is an oral contraceptive which is non-steroidal.
Page 121 :
7. OTHER CONTRACEPTIVES, The birth control implant is a contraceptive used by the, female. They prevent pregnancy for 3-4 years., It is a tiny, thin rod about the size of a matchstick., It is implanted under the skin of the upper arm., They contain progesterone and estrogen., Their mode of action is similar to that of pills., , Implanon/ Nexplanon
Page 122 :
B. PERMANENT METHOD, The permanent birth control, method in men is called, vasectomy and in women it is, called tubectomy., These are surgical methods,, also called sterilization., In vasectomy a small part of the, vas deferens is tied and cut, where as in tubectomy, a small, part of the fallopian tube is tied, and cut., This blocks, gamete transport, and prevent pregnancy.
Page 123 :
MEDICAL TERMINATION OF PREGNANCY, (MTP), An intentional or voluntary termination of, pregnancy before full term is called Medical, termination of Pregnancy (MTP) or induced, abortion., MTP is essential in cases of unwanted, pregnancies or in defective development of the, foetus., Safe during the first trimester of pregnancy., The defective development of foetus is, examined by amniocentesis.
Page 124 :
Amniocentesis is a process in which amniotic fluid containing, foetal cells is collected using a hollow needle inserted into the, uterus under ultrasound guidance., The chromosomes are studied to see the abnormalities in the, developing foetus., Amniocentesis is often misused to determine the sex of the, unborn child, and very often pregnancy is terminated if the sex of, the foetus is found to be female.
Page 125 :
Government of India has legalised MTP Act in 1971, with, strict conditions to avoid its misuse., Medical Termination of Pregnancy (Amendment) Act 2017, under section 3 of the MTP Act 1971 was enacted by, Government of India., The intention of MTP Act is to reduce the incidence of illegal, abortion and consequent maternal mortality., As per the provisions of the MTP Act, only the consent of, woman whose pregnancy is being terminated is required., According to MTP Act pregnancy may be terminated :, 1. Within first 12 weeks., 2. More than 12 weeks but lesser than 20 weeks., The registered medical practitioner’s opinion is mandatory, stating the continuation of the pregnancy would involve a, risk to the life of the pregnant woman or grave abnormal, physical or mental health or is substantial risk to the child.
Page 126 :
SEXUALLY TRANSMITTED, DISEASES (STDS), Diseases or infections, which are transmitted, through sexual intercourse, are collectively called, Sexually Transmitted, Diseases (STDs) or, Venereal Diseases (VDs) or, Reproductive Tract, Infections (RTI)., The major venereal, diseases are syphilis and, gonorrhoea., , Syphilis, Gonorrhoea
Page 128 :
INFERTILITY, It is the inability to conceive naturally after (one year of), regular unprotected intercourse., Causes of infertility could be physical, congenital,, diseases, immunological or psychological., The common physical causes in females are poly-cystic, ovary syndrome (PCOS), hormonal imbalance,, endometriosis., In male, it is less sperm count & poor quality of sperm., Prior to 1978, infertile couple had two options, adopt or, be childless., Today infertile couple have many options to have a child, such as fertility drugs, test tube babies, artificial, insemination, IUI, surrogate motherhood, etc.
Page 129 :
The childless couple can now be assisted to have babies by special, techniques known as Assisted Reproductive Technologies (ART)., , IVF (In vitro fertilization), In this process an egg is, combined with sperm, outside the body in a test, tube or glass plate to form a, zygote under simulated, conditions in the lab., The zygote or early embryos, (up to 8 blastomeres) is then, transferred into the, fallopian tube for further, development.
Page 130 :
ZIFT (Zygote Intrafallopian Transfer), ZIFT is an infertility treatment used, when there is a blockage in the, fallopian tubes which prevents the, fertilization of egg by the sperm., In this method, egg is removed from, woman’s ovary., Fertilization of the egg with sperms, is done outside the body under, sterile conditions by the process, called in vitro fertilization., The zygote is then transferred to, fallopian tube for further, development.
Page 131 :
GIFT (Gamete Intra-fallopian Transfer), Transfer of an ovum collected from a donor into the, fallopian tube of another female who can provide, suitable environment for its fertilization and, development., This technique has been developed for the cases in, which only the entrance to the oviducts or the, upper segment of the oviducts is blocked., In this procedure ova and sperms are directly, injected into regions of the oviduct, where, fertilization produces a blastocyst, which enters the, uterus via the normal route., GIFT has a success rate of about 30 percent.
Page 132 :
ICSI (Intra Cytoplasmic Sperm Injection), ICSI is an in-vitro fertilization procedure in which a single sperm, cell is injected directly into cytoplasm of an ovum in laboratory., Here the sperm has to naturally penetrate the egg., Artificial Insemination (AI), In some infertility cases, the male partner is unable to inseminate, the female due to a very low sperm count., In this, sperms are collected from the male and artificially, introduced into the cervix of female, for the purpose of achieving a, pregnancy through in-vivo fertilization (inside the body)., , IUI (Intra Uterine Insemination), This process is somewhat like that of artificial insemination, the, only difference is that the sperms are introduced into the uterine, cavity instead of cervix.
Page 133 :
SPERM BANK / SEMEN BANK, A sperm bank or semen bank is a place which, collects, stores and provides human, sperms/semen., The semen is provided by healthy males called, sperm donors., The sperms are stored in sperm bank by, cryopreservation method (at low, temperature).
Page 134 :
ADOPTION, Adoption is a legal process by which a, couple/single parent gets legal rights, privileges, and responsibilities that are associated to a, biological child for the upbringing of the, adopted child., An adoptive parent should be medically fit and, financially able to take care of the adopted, child., A person wishing to adopt a child must be at, least 21 years old. There is no legal upper age, limit for adoption